FRACTURILE DE GLEZNA
HISTORICAL REVIEW
Evidence of healed ankle fractures has been described in the remains of mummies from ancient Egypt.113 In the 5th century B.C., Hippocrates163 recommended that closed fractures be reduced by extension (traction) of the foot but that open fractures should not be reduced or the patient would die of 'inflammation and gangrene' within 7 days. Except for the anatomical descriptions of the ankle by Vesalius and a discussion of fractures of the fibula by Paré,303 there were few advances in the understanding and treatment of ankle injuries until the mid-18th century.171,215 The writings during this time show that ankle fractures, often called luxations, resulted in a high incidence of deformity and loss of function; some even thought that these 'violent luxation fractures' could be cured only by primary amputation.108
Petit307 wrote that the talus may luxate, but always in connection with a fracture or diastasis of the malleoli. He recommended careful positioning of the foot to improve the outcome. In 1768, Percival Pott312 described a fracture of the fibula 2 to 3 inches above the distal tip, with an associated rupture of the medial ligaments and lateral subluxation of the talus. Although his description and illustrations did not show an injury to the syndesmotic ligaments (always present in this injury pattern), his works are among the first to emphasize the importance of anatomical reduction in the treatment of ankle fractures. He recommended that the knee be flexed to relax the calf muscles, allowing reduction with minimal traction.
Although the literature over the next 200 years represents gradual progress in the understanding of ankle injuries, many of these reports contain conflicting information. There are differences in the terminology used to describe the anatomy, mechanism of injury, and resulting injury patterns. The same fracture pattern may be attributed to different mechanisms of injury or described in different terms, sometimes incorrectly, by different authors.171 Eponyms abound, and in some instances, this recognition is incorrectly attributed. Nevertheless, many of these observations are surprisingly accurate, considering that prior to the 20th century they were made without the benefit of radiography or surgical observation.
In 1771, Jean-Pierre David95 was the first to try to explain the mechanism of injury in fractures of the ankle. He wrote that the ligaments that held the fibula in combination with outward movement of the foot (external rotation) resulted in a fracture of the distal fibula.
Boyer the personal physician of Napoleon, described two different mechanisms of fractures of the fibula. He recognized that for subluxation of the joint to occur, there must be a malleolus fracture, a ligamentous injury, or both. This work is very likely to have influenced one of Boyer's students, Baron Dupuytren.
Dupuytren106 was the first to use experimental methods in the study of ankle injuries by producing fractures in cadavers. His writings include a combination of these experimental results and clinical observations and personal opinions. He emphasized the role of abduction and the position of the foot in the mechanism of ankle injuries and described the same fracture pattern as Pott, but included the injury to the syndesmosis.
In 1822, Astley Cooper85 presented his extensive work on fractures and dislocations, and categorized a wide range of ankle injuries, including fractures of the anterior and posterior tibial margins and diastasis of the tibia and fibula (Fig. 31-1).
![]()
Fig. 31-1
Although ignored in his own time, Maisonneuve247 was the first to compare the ankle to a mortise and tenon joint and to recognize the importance of both external rotation forces and the syndesmotic ligaments in determining the pattern of fracture. He noted that external rotation produced two different types of fractures of the fibula. When the syndesmotic ligaments remained intact, an oblique fracture occurred at the level of the joint; if the anterior tibiofibular ligament ruptured first, a proximal fibula fracture then occurred (Fig. 31-2). Although the distal fibula fracture is more common, Maisonneuve's name is associated with the proximal fracture. His work was later confirmed by the experimental studies of Huguier.172
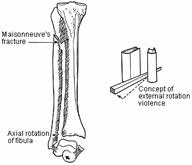
Fig. 31-2
Von Volkmann385 described a fracture of the anterior lateral portion of the tibia but incorrectly described the mechanism of injury. Tillaux375 attempted unsuccessfully to refute the work of Maisonneuve and succeeded only in incompletely describing an avulsion fracture of the lateral tibia (fragment troisičme) previously noted by Cooper.85 The same injury to the posterolateral tibia was also later described by Chaput75 and has been called the fracture of Tillaux-Chaput (Fig. 31-3). Wagstaffe387 described an avulsion fracture of the anterior margin of the fibula at the insertion site of the anterior tibiofibular ligament. This injury was also described by LeFort226 as well as others and has been called the LeFort-Wagstaffe fracture (Fig. 31-4).
Fig. 31-3

Fig. 31-4
A fracture of the posterior tibial margin was first described in 1822 by Cooper85 and then by Earle Malgaigne,248 and Chaput.75 Cotton87 later described this same fracture in the American literature, and Henderson161 subsequently called it a trimalleolar fracture.
At the beginning of this century radiographs became available. The subsequent literature contains many reports that try to correlate clinical and radiographic findings; to define mechanisms of injury, classification systems, and treatment principles; and to quantify results.196
The unsatisfactory results of closed treatment in some fractures, the availability of x-rays and anesthesia, and an increased awareness of the principles of surgical asepsis contributed to an interest in operative treatment of ankle injuries.171 In 1894, Lane209 was the first to recommend operative treatment to achieve an anatomical reduction of the ankle (Fig. 31-5). Lambotte207 wrote extensively on open reduction and internal fixation of fractures, a technique that he recommended for displaced ankle fractures (Fig. 31-6). Danis92 recommended a similar concept of internal fixation; the original anatomy of the bone was restored and maintained with stable fixation that allowed immediate movement of the involved joint and adjacent muscles.
Surgery was still generally considered only for failures of closed reduction, despite the number of unsatisfactory results with closed treatment of displaced fractures.44,60,76,204,246,264,391 Surgery was often limited only to the medial side of the ankle to provide a stable pillar for better closed reduction.98,183,196,234,264,265,368,384 Technical errors and failure to understand and restore the anatomy of the joint led to infection, implant problems, poor results, and skepticism as to the value of internal fixation.
The AO group, formed in 1958, began
a systematic study of fracture treatment.8 They
expanded the principles of Lane, Lambotte, and Danis and developed new implants
and techniques of fixation that form the basis of current operative management
of ankle fractures. Even though the group's results were good, these principles
were slow to gain acceptance in the
Recent advances have reemphasized the importance of soft-tissue management and the concept of 'biological fixation' with the use of indirect reduction techniques, limited internal fixation, and combinations of internal and external fixation for the treatment of both closed and open fractures.64,256 Biological manipulation of fracture healing and alternative methods of fixation, such as biodegradable implants and 'nonimplant' fixation, hold promise, provided the basic principles of fracture care are not forgotten.
ANATOMY
The ankle is a complex joint consisting of functional articulations between the tibia and fibula, tibia and talus, and the fibula and talus, each supported by a group of ligaments. The tibia and fibula form a mortise, providing a constrained articulation for the talus or tenon. The articular surface of the distal tibia (tibial plafond) and the mortise is wider superiorly and anteriorly to accommodate the wedge-shaped talus. The shape of the joint alone provides some intrinsic stability, especially in weight bearing (Fig. 31-7).147,261,367
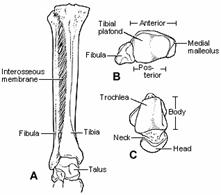
Fig. 31-7
Bone
The medial malleolus is an extension of the distal tibia. The inner surface is covered with articular cartilage and articulates with the medial facet of the talus. The distal, inner surface of the malleolus is divided by a longitudinal groove into a large, anterior colliculus and a smaller, posterior colliculus, each an attachment site for a portion of the deltoid ligament. There is also a groove on the posterior surface where the posterior tibial tendon passes behind the malleolus and the tendon sheath is attached.
The fibula provides the lateral support of the ankle. Just above the ankle joint, the fibula sits in a groove formed by a broad anterior tubercle and a smaller posterior tubercle of the tibia. There is no articular surface between the distal tibia and fibula, even though there is a small amount of motion between these two bones. The medial border of the fibula is covered by articular cartilage from the level of the tibial plafond to a point approximately halfway down its remaining length. The distal end is tapered and has a posterior groove for the peroneal tendon.
The talus has a curved head, an intermediate neck portion, and a large trapezoidal body. It articulates with the navicular, calcaneus, tibia, and fibula. The body of the talus is almost entirely covered by articular cartilage. The superior surface is convex from front to back and slightly concave from side to side. The dome of the talus is trapezoidal, and its anterior surface is an average of 2.5 mm (range, 0 to 6 mm) wider than the posterior surface.147 The articular surfaces of the malleoli are also wider anteriorly and support the talus. The medial and lateral articular facets of the talus are continuous with the superior articular surface, and the lateral facet is larger than the corresponding facet on the fibula. The majority of the talar neck has no articular surface and serves as the site of access for much of the blood supply to the rest of the talus. The multiple articular facets and lack of muscular attachments are evidence of the intercalary role of the talus in connecting the leg to the foot.
Ligaments
Stability of the ankle joint is due to a combination of the bony architecture, the joint capsule, and the ligaments. Three distinct groups of ligaments support the ankle joint: the syndesmotic, medial collateral, and lateral collateral ligaments.249
The syndesmotic ligament complex maintains the integrity between the distal tibia and the fibula and resists the axial, rotational, and translational forces that attempt to separate these two bones.321 It is made up of four ligaments: (1) the anterior tibiofibular ligament, (2) the posterior tibiofibular ligament, (3) the transverse tibiofibular ligament, and (4) the interosseus ligament (Fig. 31-8).
The anterior tibiofibular ligament originates on the anterior tubercle and anterolateral surface of the tibia and runs obliquely to the anterior fibula. The posterior tibiofibular ligament originates on the posterolateral tubercle of the tibia and inserts on the posterior fibula. It is stronger and thicker than its anterior counterpart. Because of this difference, torsional or translational forces usually cause an avulsion fracture of the posterior tibial tubercle, leaving the posterior ligament intact, while the weaker anterior tibiofibular ligament usually ruptures.
Fig. 31-8
The transverse tibiofibular ligament is often considered part of the posterior tibiofibular ligament complex and acts to deepen the posterior aspect of the ankle joint. The interosseus ligament is an extension of the interosseous membrane and is the key transverse stabilizer of the tibiofibular articulation. The ligament is triangular with a proximal apex and a broad distal base and is thinner in its midportion because of a perforating synovial pouch from the ankle joint. The interosseous membrane runs between the tibia and fibula to the level of the proximal tibiofibular joint. It stabilizes the fibula, provides additional attachment sites for muscles, and may have some load-bearing function.273
The medial ligamentous support of the ankle is provided by the superficial and deep deltoid ligaments (Fig. 31-9). The superficial deltoid ligament originates primarily from the anterior colliculus of the medial malleolus and extends in three bands to the navicular and along the plantar calcaneonavicular (spring) ligament, to the sustentaculum tali of the calcaneus, and to the medial tubercle of the talus.302 The tibionavicular portion suspends the spring ligament and prevents inward displacement of the head of the talus, while the tibiocalcaneal portion prevents valgus displacement. The superficial deltoid is also partially covered by tendon sheaths and crural fascia.
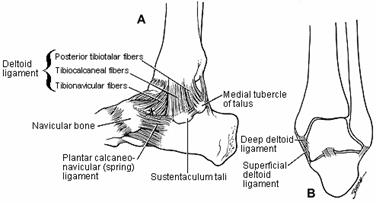
Fig. 31-9
The deep deltoid ligament originates on the posterior border of the anterior colliculus, the intercollicular groove, and the posterior colliculus.302 It is oriented transversely and inserts into the entire nonarticular surface of the medial talus. The deep deltoid extends the function of the medial malleolus and prevents lateral displacement of the talus.
The fibular collateral ligament is made up of three separate structures (Fig. 31-10). They are not as strong as the medial ligaments, because lateral support for the ankle is also provided by the fibula.
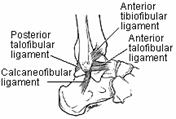
Fig. 31-10
The anterior talofibular ligament is the weakest of these ligaments. It connects the anterior fibula to the neck of the talus and prevents anterior subluxation of the talus when the ankle is in plantarflexion. The midportion of this ligament is confluent with the capsule of the ankle. This area overlies a ridge formed by the anterior border of the lateral articular facet of the talus and may be injured by this ridge with the ankle in a plantarflexed position.
The calcaneofibular ligament connects the distal fibula to a small tubercle on the posterior and lateral aspect of the calcaneus. This ligament is not associated with either the ankle capsule or the peroneal tendon sheath. It is lax in the normal, standing position, owing to the relative valgus orientation of the calcaneus. It acts primarily to stabilize the subtalar joint and limit inversion.
The posterior talofibular ligament arises from the nonarticular surface of the posteromedial fibula and inserts onto the lateral tubercle of the talus. It is the strongest of the lateral ligaments and prevents posterior and rotatory subluxation of the talus.
Tendons and Neurovascular Structures
Thirteen tendons, two major arteries and veins, and five nerves cross the ankle joint (Fig. 31-11).168 The tendons are divided into four groups. The Achilles and plantaris tendons lie posteriorly in the midline and are not intimately associated with the ankle joint. The tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles are innervated by the tibial nerve. Their tendons pass posterior to the medial malleolus, held in position by the flexor retinaculum. The tibialis anterior, extensor digitorum longus, extensor hallucis longus, and peroneus tertius muscles are innervated by the deep peroneal nerve. Their tendons pass anterior to the ankle joint and are held in position by the thick, broad extensor retinaculum. The peroneus longus and brevis muscles are innervated by the superficial peroneal nerve, and their tendons are held in position behind the fibula by the peroneal retinaculum and peroneal tendon sheath.

Fig. 31-11
The anterior neurovascular bundle (anterior tibial artery and deep peroneal nerve) crosses the ankle beneath the extensor retinaculum between the tibialis anterior and the extensor hallucis longus tendons. The posterior neurovascular bundle (posterior tibial artery and tibial nerve) passes behind the medial malleolus within the flexor retinaculum, between the flexor digitorum longus and flexor hallucis longus tendons. Three superficial sensory nerves cross the ankle. The saphenous nerve passes anterior to the medial malleolus, along with the long saphenous vein, and innervates the medial part of the foot. The superficial peroneal nerve is located just lateral to the anterior midline and supplies the skin of the dorsum of the foot. The sural nerve passes posterior to the fibula, along with the short saphenous vein, and supplies the non-weight-bearing lateral skin.
SURGICAL APPROACHES TO THE ANKLE
Adequate surgical exposure of the ankle can be obtained without injury to these structures.168 Most of these structures are superficial in the region of the ankle, and knowledge of their location is essential to prevent injury.
Anterior Approach
The anterior approach is centered between the malleoli (Fig. 31-12). It is used for anterior lip fractures of the tibia, for an arthrotomy of the joint to drain an infection or remove loose bodies, and in a limited fashion for percutaneous placement of screws. The cutaneous branches of the superficial peroneal nerve should be identified and protected. The extensor retinaculum and the location of the anterior neurovascular bundle is identified. The retinaculum is split, and the plane of dissection is either between the extensor digitorum and hallucis tendons with medial retraction of the extensor hallucis tendon and adjacent neurovascular bundle, or medial to the tibialis anterior tendon with lateral retraction of both the tibialis anterior tendon and neurovascular bundle. The ankle capsule and the joint are then exposed.
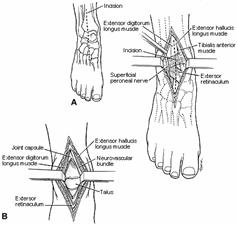
Fig. 31-12
Medial Approach
The medial approach to the ankle is centered on the malleolus itself and may be shifted either anteriorly for better access to the joint or posteriorly to expose the back of the tibia (Fig. 31-13). The incision may be longitudinal or curved distally, depending on the exposure needed. Branches of the saphenous nerve and long saphenous vein lie in the superficial tissues just anterior to the malleolus and should be protected. The dissection should be kept on the bone to prevent injury to the posterior structures, especially the tibialis posterior tendon, which is easily lacerated during exposure of the posterior aspect of the malleolus.
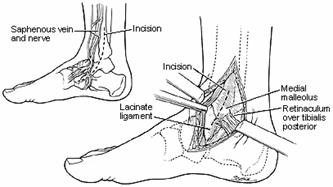
Fig. 31-13
The posterior aspect of the tibia can be exposed by dissection along the back of the malleolus and across the posterior tibia. The tibialis posterior muscle, flexor digitorum muscle, neurovascular bundle, and flexor hallucis muscle are elevated as a group and gently retracted medially or posteriorly.
Lateral Approach
The lateral approach to the ankle is used for treatment of lateral collateral ligament injuries, fractures of the fibula, injuries to the anterior or posterior syndesmosis, and reconstructive procedures (Fig. 31-14). The incision is either anterolateral or posterolateral to the subcutaneous lateral border of the fibula and can be curved distally around the tip of the fibula. The short saphenous vein and sural nerve lie posterior and the superficial peroneal nerve lies anterior to this incision. If the incision is extended proximally, the dissection is between the peroneus tertius anteriorly and the peroneus longus and brevis posteriorly.
The posterior tibia can be exposed by dissection behind and around the peroneal tendons. It is usually not necessary to remove these tendons from their sheath or divide the retinaculum.
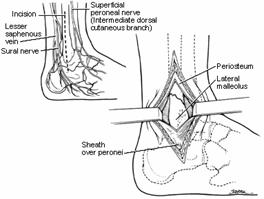
Fig> 31-14
Posterior Approach
This approach is used primarily for reconstructive procedures on the ankle or subtalar joint. The patient is prone, and a longitudinal incision is made on either side of the Achilles tendon. The retinaculum and tendon sheath should not be disturbed. The dissection is between the peroneal muscles and the flexor hallucis, exposing the posterior surface of tibia and the joint capsule or capsules.
BIOMECHANICS
The ankle functions in combination with the other joint segments of the lower limb (pelvis, hip, knee, and foot) to move the center of mass of the body as effectively as possible with a minimum expenditure of energy. The ankle-foot segment provides support and a stable but mobile base needed to maintain an upright posture. It also helps absorb the loading forces of walking, facilitates 'push-off,' and accommodates both the rotation of the limb segments above and uneven terrain below the ankle joint.174,277,412
In normal walking, the ankle is in plantarflexion as the heel contacts the ground and the weight of the body is accepted by the foot. During stance phase, the ankle initially dorsiflexes as the body moves forward over the foot, and then plantarflexes as the foot pushes off. The ankle then dorsiflexes again to help clear the foot during the swing phase. Motion analysis studies have shown that a minimum of 10° of dorsiflexion and 20° of plantarflexion are needed for this ankle function during walking.174
In the past, the ankle was considered to be a hinge joint moving about a cylindrical axis. This theory would require the malleoli to separate in dorsiflexion and narrow in plantarflexion to accommodate the shape of the talus while maintaining stability. However, more recent studies have shown that the amount of separation of the malleoli during ankle motion ranges from 0.2 to 1.8 mm with weight bearing and from 0 to 1.6 mm during non-weight-bearing ankle motion.147 Most of this change occurs as the ankle moves from full plantarflexion to neutral with less change from neutral to dorsiflexion. By computed tomography (CT) the joint remains congruous with no change in the relationship of the malleoli and the talus in different ankle positions.238 Michelson and colleagues272 reported that the talus may translate laterally up to 2 mm after simple axial loading.
Inman,174 correlating the anatomy and function of the ankle, described the joint as shaped like part of a cone, with the apex of the cone directed medially toward the medial malleolus and the base of the cone directed laterally toward the distal fibula. The axis of the cone corresponds to the mechanical axis of the joint and extends posterolateral from just below the medial malleolus to the tip of the lateral malleolus. This axis is rotated 20° to 30° external to the axis of the knee and in the frontal plan is aligned 80° to the long axis of the tibia. Although the actual center of rotation moves slightly during the arc of rotation, for most clinical purposes the axis of motion can be considered to run between the distal tips of the malleoli. The malleoli act as pillars for attachment of the ligaments close to the axis of rotation of the joint.261 This enables some portion of the medial and lateral ligament complex to remain tight throughout the arc of flexion and extension and thereby provide rotational stability.
The stability of the ankle is primarily dependent on four groups of bony and ligamentous structures: (1) medial malleolus and medial collateral ligaments, (2) lateral malleolus and lateral collateral ligaments, (3) anterior syndesmotic ligaments and their bony attachment sites on the tibia and fibula, and (4) posterior syndesmotic ligament and posterior malleolus. Tile374 has emphasized that there is a spectrum of instability, dependent on the degree of soft-tissue and skeletal injury. If only one of the above groups is injured, stability will be maintained. As each successive group of structures is injured, the ankle becomes more unstable.
A number of experimental studies have been performed to evaluate the effect of bone and ligament 'injury' on the stability of the ankle joint. Variations in testing methods, alteration of the normal anatomy of the ankle and foot to facilitate testing, and application of forces in a single plane or at less than physiological load have resulted in some conflicting data and difficulty in correlating some experimental results with clinical observations.
The contribution of individual ligaments to ankle stability has been studied using serial sectioning techniques.80 If only the syndesmotic ligaments are divided, but the fibula, lateral collateral ligaments, and the deltoid remain intact, there is no widening of the mortise. If both the syndesmosis and fibula are disrupted, the talus can shift laterally 2 to 3 mm, even with the deep deltoid ligament intact. Further displacement indicates that either the deep deltoid ligament or the medial malleolus must be disrupted. Rotational stability of the ankle results from the congruency of the articular surfaces and the functional orientation of the supporting ligaments, which are both enhanced during weight-bearing (vertical loading).237
In the lower limb, up to one sixth of the weight is carried by the fibula and the rest by the tibia.206 The fibula is pulled distally in stance phase by the action of the long toe flexors; the interosseous membrane is tightened, the mortise deepened, and the fibula pulled slightly medially, resulting in increased rotational stability for the ankle.344,396
The weight-bearing contact area of the ankle is relatively large compared with the hip or knee, owing to the high congruence of the articular surfaces. Displacement of the talus leads to incongruence, which decreases the contact surface area and increases the stresses over the remaining contact areas. Ramsey and Hamilton318 reported that a 1-mm lateral shift of the talus decreased the contact area by 42%; with 3 mm of lateral shift, the contact area decreased by more than 60%. The fibula is essential in providing stability and preventing displacement of the talus. A shortened or malrotated fibula will allow the talus to shift or tilt even if the medial ligaments are intact.416 Because even small changes significantly influence the joint contact area, restoration of the anatomy of the fibula and consequently the ankle joint is important.
How anatomical must the reduction be for a good result? Neither clinical nor biomechanical studies give absolute values, and there are recommendations ranging from mandatory anatomical reduction to an acceptable displacement of 2 to 3 mm. Regardless of treatment bias, all the referenced articles for this chapter are in agreement that outcome correlates with the ability to achieve and maintain reduction of the ankle and that the incidence of unsatisfactory results increases as residual displacement exceeds 3 mm.
MECHANISMS OF INJURY
The pattern of injury to the ankle depends on many factors, including the age of the patient, the quality of the bone, the position of the foot at the time of injury, and the direction, magnitude, and rate of the loading forces. Although many individuals have contributed, much of our current understanding of the mechanisms of ankle injury is derived from the work of Lauge-Hansen.216,217,218, 219,220 He emphasized the influence that the position of the foot had on the injury pattern and correlated this position with the direction of the deforming forces. In his system, the position of the foot (pronation or supination) at the time of injury is described first and the direction of the deforming force is described second. The common deforming forces acting on the ankle are adduction, abduction, external rotation, and vertical loading (Fig. 31-15). As clarified by Pankovich pronation and supination refer to the position of the foot as it rotates around the axis of the subtalar joint. Adduction and abduction are deforming forces resulting in rotation of the talus around its long axis, while internal and external rotation are rotational movements around the vertical axis of the tibia. The mechanisms of injury are described using this terminology.
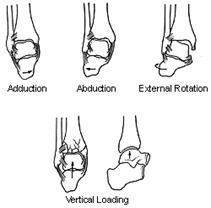
Fig> 31-15
Supination-Adduction
As the foot supinates, the lateral structures tighten (Fig. 31-16). Continued supination and adduction force may rupture portions of the lateral collateral ligaments or avulse these ligaments from their bony attachment sites on the distal fibula, resulting in an ankle sprain. Alternatively, the distal fibula may be avulsed, resulting in a transverse fracture below the level of the intact syndesmotic ligaments. Further adduction drives the talus against the medial side of the joint, resulting in a vertical fracture of the medial malleolus and sometimes an impaction fracture of the medial articular surface of the tibia. These forces can also result in an impaction or osteochondral fracture of the talus or injury to its articular surface.23
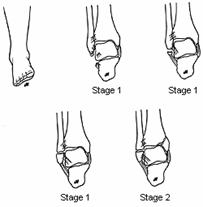
Fig. 31-16
Supination-External Rotation
As the supinated foot externally rotates (or the leg internally rotates on the planted, supinated foot), the lateral structures and anterior syndesmotic ligaments tighten (Fig. 31-17). The anterior syndesmosis is usually injured with either rupture of the ligament or avulsion of its bony insertion or insertions. External rotation produces a spiral fracture of the fibula, which runs anteroinferior to posterosuperior. The fracture may begin below, at, or above the attachment site of the anterior tibiofibular ligament on the anterior tubercle of the fibula.150 If the fracture begins below the anterior tubercle of the fibula, the anterior tibiofibular ligament remains intact. The fracture passes obliquely through the superior articular surface of the fibula. Most commonly, the fracture begins at or just above the level of the anterior tubercle, and the anterior syndesmosis is partially or completely disrupted. Rarely, the supination-external rotation pattern may be present in fibula fractures occurring above the level of the syndesmosis, with disruption of both the syndesmosis and interosseous membrane.300 With continued force, the rotating talus may put tension on the posterior syndesmosis, resulting in either rupture of the posterior tibiofibular ligament or, more commonly, an avulsion of the posterior lateral tubercle. In some instances the fibula fracture may, in effect, decompress these structures, so that the force of the talus is directed medially and no posterior injury occurs. Finally, if sufficient force remains, there is tension on the medial structures, resulting in either an avulsion fracture of the medial malleolus or rupture of the deltoid ligament. With this medial injury, the talus is free to shift laterally.
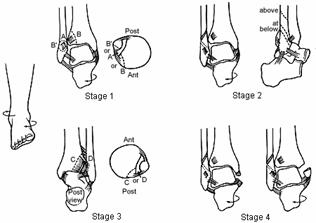
Fig. 31-17
Pronation-Abduction
 In pronation, the medial structures tighten and are injured first
(Fig. 31-18). There is either an avulsion fracture of the medial malleolus or
rupture of the deltoid ligament. The abduction force then either ruptures the
syndesmotic ligaments or avulses their bony attachment sites. Continued lateral
force from the talus fractures the fibula at or above the level of the
syndesmosis and ruptures the interosseous membrane up to the level of this
fracture. This fracture results from bending and is either oblique or partially
transverse with lateral comminution or a butterfly fragment. This fibular
fracture pattern signals an associated medial injury.
In pronation, the medial structures tighten and are injured first
(Fig. 31-18). There is either an avulsion fracture of the medial malleolus or
rupture of the deltoid ligament. The abduction force then either ruptures the
syndesmotic ligaments or avulses their bony attachment sites. Continued lateral
force from the talus fractures the fibula at or above the level of the
syndesmosis and ruptures the interosseous membrane up to the level of this
fracture. This fracture results from bending and is either oblique or partially
transverse with lateral comminution or a butterfly fragment. This fibular
fracture pattern signals an associated medial injury.
Fig. 31-18
Pronation-External Rotation
The medial side is injured first. External rotation then results in rupture of the anterior tibiofibular ligament or its bony insertion, followed by fracture of the fibula at or above the syndesmosis (Fig. 31-19). The fibular fracture is spiral, but runs anterosuperior to posteroinferior, and the interosseous membrane is ruptured up to the level of the fibula fracture.290,298,300 With continued rotation the posterior syndesmosis is injured, with either rupture of the ligament or an avulsion fracture of the posterolateral tibia.
Fig> 31-19
Proximal fractures of the fibula (Maisonneuve-type) result from external rotation.300 There are variations in the pattern of the fibula fracture, reflecting either a supination-external rotation or pronation-external rotation type of injury. The foot may even move from relative pronation to supination during the injury.
Vertical Loading
Vertical loading drives the talus into the distal tibia. The position of the foot and the rate of loading affect the injury pattern, which can range from isolated fractures of the anterior or posterior lip of the tibia to complex, intra-articular fractures of the distal tibia (pilon fracture) (Fig. 31-20).
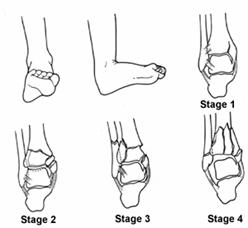
Fig. 31-20
Summary
Injuries to the ankle result in many different combinations of bone and ligament injury. The position of the foot influences the location of the initial stage of injury: supination of the foot tightens the lateral structures, which are injured first; pronation tightens the medial structures, which then will be injured first. The injury pattern then moves sequentially around the ankle in the same direction as the deforming force.
On the lateral side, adduction results in injury to the lateral collateral ligament or avulsion of the distal fibula. Abduction causes a bending fracture, often with comminution, while external rotation produces a characteristic spiral fracture. Injury to the syndesmotic ligaments should be suspected when the fibula is fractured at or above the level of the syndesmosis.
The injury to the medial side results either from a direct impact of the talus or from tension as the talus rotates or moves laterally following the fibula. Several combinations are possible301: the deep deltoid ligament can be torn, leaving the malleolus intact. The anterior colliculus may be avulsed by the superficial deltoid, leaving the deep deltoid ligament either intact or ruptured. Avulsion of the posterior colliculus is uncommon and often associated with a long, posteromedial spike of bone. Finally, a fracture above the level of the ligamentous attachment leaves the deltoid ligament attached to the distal malleolar fragment.
Fractures of the posterior malleolus are caused by abduction or external rotation, posterior displacement of the talus, vertical loading, or combinations of these forces. In external rotation or abduction, the posterior tibiofibular ligament is under tension and can either rupture or, more commonly, avulse the posterolateral corner of the tibia (Volkmann's triangle). The posterior or posteromedial malleolus can be fractured by direct impact of the talus as it rotates or is driven against the posterior malleolus, as may occur in a posterior fracture-dislocation or from an associated axialloading, vertical shear type of injury.
Syndesmotic disruption occurs from external rotation or abduction forces. The ligaments rupture or avulse their bony insertions. The fibula may be intact but is usually fractured at or above the level of the injured syndesmosis. In more extensive injuries, the portions of the interosseous membrane may be torn distally to proximally and a proximal fibula fracture may be present.
These mechanisms account for most ankle injuries. It is difficult to re-create, even in an experimental setting, all of the variables involved in producing an injury, including the dynamic forces of muscles, different magnitudes and rates of loading, different degrees of weight bearing, and differences in the quality of bone and soft tissues. These factors may account for some of the variations within these general groups of mechanisms of injury and also for those few fractures that do not conform to any one of these patterns.
CLASSIFICATION
A classification system is useful only if it assists in the selection of the appropriate management, offers a prognosis of eventual outcome, or allows comparison of the results of treating similar injuries. Many different classification systems have been reported, each based on combinations of clinical, experimental, and radiographic criteria, with some systems also incorporating assessment of mechanisms of injury, bone and ligament injury, and joint stability.11,34,91,92,161,216,217, 218,219,220,392,393 Several different classification systems of ankle injuries are in use.
Henderson161 presented a classification based on radiographic findings that separated injuries into three groups: isolated fractures of the medial, lateral, posterior, or anterior malleolus; bimalleolar fractures; and trimalleolar fractures. This is a simple, descriptive system that is commonly used.
Lauge-Hansen System
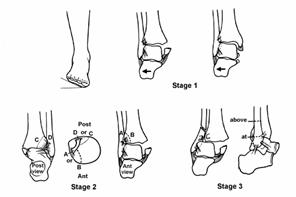
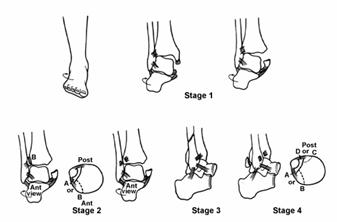
The Lauge-Hansen classification is based on experimental, clinical, and radiographic observations.216,217,218, 219,220 He found that injuries occurred in a sequential manner, which he separated into stages. In this system the position of the foot (pronation or supination) at the time of injury is described first and the direction of the deforming force second. More than 95% of ankle injuries can be placed in one of the four groups.413 The terms eversion and inversion as used by Lauge-Hansen are the same as external rotation and internal rotation of the foot. A fifth group, pronation-dorsiflexion, was later added to account for fractures caused by axial loading. Each of these groups has several stages of injury, which are listed in Table 31-1 (see Fig. 31-16, Fig. 31-17, Fig. 31-18, Fig. 31-19 and Fig. 31-20).
TABLE 31-1
Lauge-Hansen Classification*
SUPINATION-ADDUCTION (SA)
Transverse avulsion-type fracture of the fibula below the level of the joint or tear of the lateral collateral ligaments
Vertical fracture of the medial malleolus
SUPINATION-EVERSON (EXTERNAL ROTATION) (SER)
Disruption of the anterior tibiofibular ligament
Spiral oblique fracture of the distal fibula
Disruption of the posterior tibiofibular ligament or fracture of the posterior malleolus
Fracture of the medial malleolus or rupture of the deltoid ligament
PRONATION-ABDUCTION (PA)
Transverse fracture of the medial malleolus or rupture of the deltoid ligament
Rupture of the syndesmotic ligaments or avulsion fracture of their insertion (s)
Short, horizontal, oblique fracture of the fibula above the level of the joint
PRONATION-EVERSION (EXTERNAL ROTATION) (PER)
Transverse fracture of the medial malleolus or disruption of the delotid ligament
Disruption of the anterior tibiofibular ligament
Short oblique fracture of the fibula above the level of the joint
Rupture of posterior tibiofibular ligament or avulsion fracture of the posterolateral tibia
PRONATION-DORSIFLEXION (PD)
Fracture of the medial malleolus
Fracture of the anterior margin of tibia
Supramalleolar fracture of the fibula
Transverse fracture of the posterior tibial surface
* Classification groups with injury stages.
Danis-Weber System
 The Danis-Weber279,392,393 system is based
on the level of the fracture of the fibula. The more proximal
the fracture of the fibula, the greater the risk of injury to the syndesmosis
and the more likely that the joint will be unstable. There are three
types of fractures in this classification system.
The Danis-Weber279,392,393 system is based
on the level of the fracture of the fibula. The more proximal
the fracture of the fibula, the greater the risk of injury to the syndesmosis
and the more likely that the joint will be unstable. There are three
types of fractures in this classification system.
Fig. 31-21
The type A injury is a fracture of the fibula occurring below the level of the tibial plafond. These are avulsion fractures resulting from supination of the foot. If this force continues, there may be an oblique or vertical fracture of the medial malleolus. The Weber 'A' fracture corresponds to the Lauge-Hansen supinationadduction injury.
The type B injury is an oblique or spiral fracture caused by external rotation. The fracture begins at or near the level of the syndesmosis. The anterior syndesmotic ligaments are partially or completely torn in about 50% of type B injuries, while the posterior syndesmotic ligaments usually remain attached to the posterior aspect of the distal fibular fragment. There may be an associated injury to the medial side of the ankle as well as to the posterior malleolus. The Weber 'B' fracture corresponds to the supination-eversion injury of Lauge-Hansen.
The type C injury is a fracture of the fibula above the syndesmosis. The syndesmosis is disrupted, and there is almost always an associated injury on the medial side of the ankle. The type C injury is divided into fractures involving the diaphysis of the fibula and the proximal fibula (Maisonneuve type). The Weber 'C' fracture corresponds to the pronation eversion or pronation abduction stage 3 injuries of Lauge-Hansen.
The AO classification of fractures has further divided each of these three types into three groups, to quantify the spectrum of injury within each type (Table 31-2; Fig. 31-21).281
TABLE 31-2
AO Classification of Malleolar Fractures*
TYPE A: FIBULA FRACTURE BELOW SYNDESMOSIS
(INFRASYNDESMOTIC)
A1-isolated
A2-with fracture of medial malleolus
A3-with a posteromedial fracture
TYPE B: FIBULA FRACTURE AT THE LEVEL OF
SYNDESMOSIS (TRANSSYNDESMOTIC)
B1-isolated
B2-with medial lesion (malleolus or ligament)
B3-With a medial lesion and fracture of posterolateral tibia
TYPE C: FIBULA FRACTURE ABOVE SYNDESMOSIS
(SUPRASYNDESMOTIC)
C1-diaphyseal fracture of the fibula, simple
C2-diaphyseal fracture of the fibula, complex
C3-proximal fracture of the fibula
* Classification into fracture type (A-C) and group (3-1)
Ankle injuries have also been further simplified and divided into three groups based on a general mechanism of injury. These groups include injuries caused by adduction-inversion (supination), resulting in a lateral injury below the syndesmosis; by external rotation-abduction, resulting in lateral injury at or above the syndesmosis; and by vertical loading, resulting in a fracture involving primarily the distal tibia (pilon fracture).
Although joint stability is implied in the LaugeHansen and Danis-Weber systems, Tile374 believed that the specific assessment of stability was an important part of treatment planning and should be included in the classification system. He subdivided adduction-inversion and external rotation-abduction injuries into stable and unstable types. This system is based on two factors: the characteristics of the injury to the lateral side of the joint and the clinical and radiologic assessment of stability.
Both Lauge-Hansen and Danis-Weber classifications are widely used, and therefore some understanding of both systems is important.235 The Lauge-Hansen system is useful because it characterizes the mechanism and sequence of injury and, in particular, emphasizes the associated ligamentous injuries. It is more complex, and all fractures do not conform exactly to one of the described patterns. In the supination- external rotation fracture, for example, the stage 1 injury is not always present, and a medial (stage 4) injury can occur without a posterior (stage 3) injury.
The Danis-Weber system is simpler, emphasizes the importance of the lateral side of the ankle, and is useful in planning surgical treatment. Initially, this system did not distinguish the extent of involvement and was too inclusive. Type B, for example, included the spectrum of supination-external rotation injuries, which do have a different prognosis. This problem has been addressed in the AO classification. The system proposed by Tile is easy to remember and emphasizes the importance of assessing and relating stability to the structures that are injured.
Ankle injuries include many variations and combinations of bone and ligament injuries. Any classification system that attempts to categorize all possible combinations will become complex and difficult to use or remember. There is some advantage in understanding these different systems, because each emphasizes features of the anatomy and pathomechanics important in evaluation and treatment planning. All of these systems require a thorough evaluation of the patient, and treatment decisions should not be made only on the basis of radiographic appearance or classification categories.
SIGNS AND SYMPTOMS
History
Patients can usually remember the event but often cannot describe the exact mechanism by which their injury occurred. The event may provide some information as to the magnitude of the injury and the likelihood of associated injuries. Vertical loading from falls or high-speed deceleration may result in axial compression injuries to the foot, ankle, and spine, while twisting usually results in an external rotation injury.
A history of prior ankle problems or injury may be important. Recurrent injuries, particularly ligament sprains, are common, and preexisting laxity, instability, or radiographic abnormalities can be misinterpreted as an acute injury. The patient's medical history should be reviewed because systemic problems such as diabetes, peripheral vascular disease, or metabolic bone disease may affect treatment planning.
Physical Examination
A careful examination is needed to determine the status of the skin, soft tissues, and neurovascular structures, as well as the bones and ligaments. The entire lower leg, including the fibula, should be examined. Combinations of tenderness, swelling, or ecchymosis over the bone, ligaments, or joint line suggest an injury. The stability of the joint should be assessed, especially when these findings are associated with normal x-rays. Based on the physical findings, an anterior drawer, inversion, eversion, or external rotation stress test may be helpful.
Stress testing is often difficult in the acute setting, and analgesic premedication and local or regional anesthesia may be needed. Although pain or tenderness over the structures being stressed suggests an injury, it is difficult to determine the extent of the injury by stress testing alone. Stress x-rays of both ankles provide an objective measurement of the instability and should be obtained at the same time.
The anterior drawer maneuver evaluates the anterior talofibular ligament. With the ankle in neutral position, a forward force is applied to the heel while a backward force is applied to the tibia. A difference of more than 8 mm compared with the opposite side suggests an injury. This test can also be done by resting the heel on a firm surface and gently pressing backward on the distal tibia.89 An inversion (supination) stress test is performed with the ankle in plantarflexion to test the anterior talofibular ligament and in neutral or slight dorsiflexion to test the calcaneofibular ligament. The ankle is inverted and comparison made to the opposite side. An eversion stress test is performed with the ankle in neutral and tests primarily the superficial deltoid ligament complex. An external rotation stress test evaluates the syndesmotic ligaments and, secondarily, the deep deltoid ligament. The tibia is stabilized, the ankle placed in a neutral position, and the foot externally rotated.
Although injury to neurovascular structures is uncommon in an ankle injury, massive swelling, particularly when associated with a crush or penetrating injury, ankle dislocation, or fracture or fractures of the tibia or foot, may compromise blood flow and result in ischemia; and compartment pressure measurements, Doppler imaging, and transcutaneous measurement of PO2 can be used along with clinical judgment to assess the vascular status and determine if decompression or other intervention is indicated.
As part of this initial evaluation, the ankle should be gently reduced and immobilized in a padded splint to prevent further soft-tissue injury and decrease swelling. Application of ice packs, elevation of the extremity, and compression are used to reduce swelling as evaluation and treatment planning proceed.
RADIOGRAPHIC FINDINGS
The standard radiographic evaluation of the ankle includes anteroposterior, lateral, and mortise views. A number of radiographic measurements can be made from these views and, if necessary, compared with the opposite side. These parameters can provide an objective measurement of instability and are useful not only in diagnosis but also in planning treatment and in assessing the accuracy of reduction and final results.144,184
The anteroposterior x-ray is taken in line with the long axis of the foot. The entire fibula should be included on this radiograph if there is any lateral tenderness above the joint line. This view is used to evaluate fractures of the medial or lateral malleolus, anterolateral tibia, proximal fibula, and osteochondral fractures of the distal tibia or talus. Assessment of articular congruity and measurements of relative malleolar length, syndesmotic integrity, and talar shift can be made (Fig. 31-22).

Fig. 31-22 A) Glezna normala. A-B Spatiul clar tibio-fibular; B-C Suprapunerea tibiofibulara
 The lateral view is
obtained with the limb perpendicular to the long axis of the foot. The dome of
the talus should be centered under the tibia and congruous with the distal
tibial articular surface. Asymmetry of this articular space, especially
anterior widening, suggests instability.343 The fibula
overlaps the posterior aspect of the tibia, but the posterior tubercle of the
tibia can still be seen. This view is used to evaluate displacement of the
talus in the anterior or posterior direction, fractures of the posterior or
anterior tibial margins, fractures of the talar neck, and fractures or
posterior dislocation of the fibula (Fig. 31-23).
The lateral view is
obtained with the limb perpendicular to the long axis of the foot. The dome of
the talus should be centered under the tibia and congruous with the distal
tibial articular surface. Asymmetry of this articular space, especially
anterior widening, suggests instability.343 The fibula
overlaps the posterior aspect of the tibia, but the posterior tubercle of the
tibia can still be seen. This view is used to evaluate displacement of the
talus in the anterior or posterior direction, fractures of the posterior or
anterior tibial margins, fractures of the talar neck, and fractures or
posterior dislocation of the fibula (Fig. 31-23).
Fig. 31-23
The mortise view is obtained with the leg internally rotated 15° to 20° so that the x-ray beam is nearly perpendicular to the intermalleolar line. The articular surface of the talus should be congruous with that of the distal tibia. The clear space (articular space) between the talus and the medial malleolus, distal tibia, and lateral malleolus should be equal. Fibular length, talar tilt, talar shift, talocrural angle, medial clear space, tibiofibular overlap, and tibiofibular clear space (interosseous clear space) can be measured (Fig. 31-24). Small osteochondral lesions may be difficult to see because of the dome shape of the talus. Mortise views as the ankle is moved from plantarflexion to dorsiflexion may show these lesions more clearly.
Radiographic Measurements of Alignment and Stability184,308
Tibiofibular Line
On the mortise view, a line formed by the subchondral bone of the distal tibia and the medial aspect of the fibula should be continuous. Disruption of this line indicates shortening, rotation, or lateral displacement of the fibula (see Fig. 31-24B).
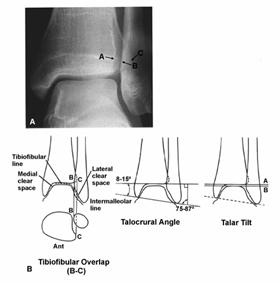
Fig. 31-24
Talocrural Angle90,184,337
The talocrural angle is formed on the mortise view by a line drawn parallel to the articular surface of the distal tibia and one connecting the tips of both malleoli (intermalleolar line). The angle is normally between 8° and 15°. Another method of measurement is to use the angle formed by a line perpendicular to the distal tibial articular surface and the intermalleolar line. This angle is normally between 75° and 87°. By either method this angle should be within 2° to 3° of the opposite side. A difference of greater than this is abnormal and indicates fibular shortening (see Fig. 31-24B).
Talar Tilt
There are several methods of measuring talar tilt on the mortise view (see Fig. 31-24B). A line drawn parallel to the articular surface of the distal tibia and a second line drawn parallel to the talar surface should be parallel to each other. Alternatively, the angle between the intermalleolar line and each of these two articular surface lines is measured. The difference between these two angles is the talar tilt.374 By either method, the normal tilt angle is 0°, with a range from -1.5° to +1.5°. On the anteroposterior view, the difference in the width of the superior clear space between the medial and lateral side of the joint should be less than 2 mm.184 These are static measurements of talar position. In a normal ankle, the talus may tilt up to 5° with an inversion stress.90 Measurements of talar tilt using stress x-rays are used to evaluate lateral ligament stability.
Medial Clear Space
On the mortise view, the distance between the lateral border of the medial malleolus and the medial border of the talus is measured. Because the articular surfaces are oblique, similar borders (anterior edge of medial malleolus to anterior talus or posterior edge of medial malleolus to posterior talus) should be used or the measurement may be incorrect.184 Normally, this space is equal to the superior clear space between the talus and distal tibia (see Fig. 31-24B). A space of greater than 4 mm is abnormal and indicates lateral shift of the talus.
Syndesmotic Integrity
The relationship between the distal tibia and fibula reflects the integrity of the syndesmotic ligaments.184,343 The fibula is posterior and lateral to the tibia, and the anterolateral portion of the tibia overlaps the fibula. On the anteroposterior view, this tibiofibular overlap is measured between the lateral border of the anterior tibial prominence and the medial border of the fibula (distance B to C; see Fig. 31-22B). An overlap of less than 10 mm is abnormal and indicates a syndesmotic injury, resulting in separation of the tibia and fibula. On the mortise view this tibiofibular overlap should be 1 mm or less (see Fig. 31-24B).
The tibiofibular clear space (interosseous clear space) is the distance between the groove formed by the anterior and posterior tubercles of the tibia and the fibula. On the anteroposterior x-ray this distance between the lateral border of the posterior tibial malleolus and the medial border of the fibula (distance A to B; see Fig. 31-22B) should be less than 5 mm. A wider space indicates a syndesmotic injury.
It should be apparent that plain x-rays of good technical quality are essential to evaluate the ankle. They define the bony anatomy and provide direct or indirect evidence of joint instability. Abnormal talar tilt (especially into valgus), increased width of the mortise, subluxation of the talus, shortening or displacement of the fibula, and fracture of the posterior malleolus are all radiographic signs that suggest instability. Persistent radiographic abnormality after treatment may indicate inadequate reduction, unrecognized instability, interposed soft tissue, or technical errors of fixation.
Specialized Evaluation
Stress X-Rays
Stress x-rays are used to confirm suspected ligamentous instability. Stress views of the opposite ankle must be obtained for comparison. To evaluate the lateral ligaments, an anteroposterior and mortise view is taken with an inversion (supination) stress on the ankle. Stress views with the foot in plantarflexion isolate the anterior talofibular ligament, while views in neutral evaluate both the anterior talofibular and calcaneofibular ligaments.212,343 There is normally less than 5° of talar tilt in the normal ankle.90 A difference in tilt of twice the uninjured ankle or a talar tilt of more than 10° to 15° indicates a tear of the anterior talofibular and calcaneofibular ligaments (Fig. 31-25). The external rotation stress x-rays evaluate the syndesmosis, and good views of the mortise are needed to make accurate measurements of syndesmotic integrity. A lateral x-ray during an anterior or posterior drawer stress may show subluxation of the talus. An anterior shift of greater than 8 to 10 mm compared with the uninjured ankle indicates a tear of the anterior talofibular ligament (Fig. 31-26).
The measurements obtained from the stress views may be influenced by the degree of patient relaxation, the position of the ankle, the amount of force used in testing, and the laxity of the contralateral ankle.
Arthrography
Arthrography has been used to evaluate the integrity of the capsule and ligaments of the ankle.51,53,190,293 Radiopaque dye is injected into the ankle joint. Extravasation anterior to the lateral malleolus indicates a tear of the anterior tibiofibular ligament. Communication of dye between the joint and the peroneal sheath after injection at either location indicates a tear of the calcaneofibular ligament. Arthrography is accurate in identifying ligamentous disruption but must be performed within 1 week, before tears in the capsule begin to heal. Stress testing, in comparison, is accurate but only when done correctly with adequate patient analgesia.176,214 Magnetic resonance imaging (MRI) has largely replaced arthrography of the ankle when cost, availability, and expertise in performing the study is considered.
Tomography
Anteroposterior and lateral tomography has been used to evaluate complex fracture patterns, especially when the distal tibia was involved (pilon fracture) or in suspected triplane fractures in adolescents. The use of conventional tomography of the ankle has largely been replaced where computed tomography with multiplanar and three-dimensional reconstruction is available.
Computed Tomography
Computed tomography is used to evaluate complex or comminuted fractures, particularly of the distal tibia or when the injury pattern is not clearly delineated by plain radiographs (Fig. 31-27).123,245 Multiplane and three-dimensional reconstructions may provide additional information. CT has also been used to help plan reconstructive procedures such as correction of malunions and to stage and monitor the healing of osteochondral defects.9,350,245
Magnetic Resonance Imaging
Magnetic resonance imaging allows multiplanar imaging without radiation. MRI is a useful diagnostic tool in the assessment of acute and chronic tendon and ligament injuries about the ankle. It has also been useful in the evaluation of subtle fractures, including osteochondral and stress fractures not evident on plain radiographs.9,195,350 An MRI examination consists of a combination of T1- and T2-weighted images in the axial, coronal, or sagittal planes. Imaging is performed with a surface coil that functions to increase the signal-to-noise ratio. T1- and T2-weighted axial images are best for diagnosing tendon or ligamentous injuries. A torn ligament may appear thickened, retracted, or discontinuous and often has a higher signal intensity than normal, appearing gray rather than black. Although ligamentous injuries of the ankle can be seen on MRI, physical examination and stress x-rays provide accurate information at much less cost. The coronal and sagittal planes are most useful for evaluating the talus. On MRI, nondisplaced and stress fractures appear as linear regions of low signal intensity that extend to the surface. An amorphous pattern of low signal intensity with T1 weighting and high signal on T2 weighting is usually seen in the adjacent marrow and soft tissues in these injuries.195
Bone Scan
Bone scans are used primarily in the evaluation of chronic ankle problems, especially in suspected osteochondral injuries, infection, stress fractures, and reflex dystrophies.
Arthroscopy
Arthroscopy of the ankle has been used in the evaluation and management of osteochondral lesions of the talus and chronic ankle problems with suspected intra-articular pathology.16,118,304,314,392 Lateral osteochondral lesions are usually shallow and are relatively easy to remove through a standard anterolateral arthrotomy, while the medial lesion is posterior on the talar dome and in the past frequently required a medial malleolar osteotomy. Detached osteochondral fragments can be removed and the craters curetted or abraded satisfactorily using arthroscopic techniques.118 Bryant and Siegel described a technique for drilling osteochondral defects using meniscal repair instrumentation through anterior portals rather than using an anterior cruciate ligament guide through a transmalleolar approach.56 The less invasive nature of arthroscopic procedures decreases postoperative morbidity and facilitates rehabilitation. In addition, the entire ankle joint can be inspected for associated signs of disease. Pritsch and associates315 found adhesions of the distal tibiofibular syndesmosis as the cause of chronic ankle pain in 11 of 19 symptomatic patients after an uncomplicated fracture of the ankle. Symptoms resolved after arthroscopic resection of the adhesions in all 11 patients. Ferkel and Fasulo120 reported 75 (84%) patients with a poor response to conservative treatment for anterolateral impingement who had good to excellent results after arthroscopic synovectomy and debridement when observed for 7 years.
There is some early experience using arthroscopy to monitor reduction of the intra-articular portion of an ankle fracture; however, the usefulness of this technique requires further evaluation. Fractures may be reduced under arthroscopic vision using Kirschner-wire joysticks to manipulate the fragments and fixed with cannulated screws though small stab incisions. Ferkel and Fasulo120 arthroscopically evaluated 22 consecutive ankle fractures. They found 68% had osteochondral lesions of the talus that were not seen on preoperative radiographs, 63% had loose bodies, and 38% had chondromalacia. Whipple and associates399 described arthroscopic management of triplane fractures of the ankle in two patients. They believed arthroscopic management reduced surgical trauma, provided a method of accurate delineation of fracture fragment orientation, and ensured accurate reduction under direct visualization.
TREATMENT
Nonoperative Treatment
The goals of treatment are to obtain an anatomical reduction, maintain this reduction until the fracture heals, and return the patient to his or her preinjury level of function with a painless, mobile ankle. Many studies have attempted to compare the results of nonoperative and operative treatment.18,19,60,76,117, 170,196,203,225,308,309,310, 328,334,380,398, 404,414,415 Similar results are reported when these goals of treatment are achieved by either method of treatment. The outcome correlates directly with how well the anatomy of the ankle has been restored. In some fracture patterns a closed reduction may be difficult to achieve or maintain. Loss of reduction and repeated manipulations have been associated with unsatisfactory results.44,60,117 Prolonged immobilization may also lead to disuse osteoporosis and joint stiffness.8,279
The indications for operative treatment and, consequently, nonoperative treatment have changed over the past 25 years. The 'good results' of the past often change with current standards and expectations.69 Closed reduction is indicated for nondisplaced or stable fractures, for displaced fractures when an anatomical reduction is obtained and maintained without repeated manipulation, and when operative treatment is not indicated because of the general condition of the patient or the leg. Closed reduction is also indicated when operative treatment is planned but will be delayed.
Technique of Closed Reduction
Successful closed reduction requires an understanding of the mechanism of injury and an assessment of the inherent stability of the injury.34,76,391,403 A closed reduction is obtained by reversing the mechanism of injury to the ankle. Good quality, postreduction x-rays are essential, and the radiographic parameters that assess stability and reduction should be carefully measured.
Avulsion fractures of the lateral malleolus (supination-adduction or Weber type A) are usually stable and minimally displaced; these do well with closed treatment.170 Eversion relaxes the lateral collateral ligaments, and the distal fibula can be reduced, if necessary. An associated oblique fracture of the medial malleolus makes closed treatment more difficult. Pronation of the foot and abduction will reduce the fracture, but it is an unstable pattern and difficult to hold. Most fractures with this pattern will require operative treatment.
External rotation fractures at the level of the syndesmosis (supination-external rotation or Weber type B) are reduced by gentle distraction, internal rotation, and varus stress. Quigley316 achieved this position by placing a stockinette over the lower leg, turning the patient with the injured side down, and then suspending the free end of the stockinette. A cast was then applied with the foot in this position. Correct casting technique and molding is essential to maintain reduction. Careful examination of the postreduction x-rays is needed because shortening and external rotation of the fibula may be subtle and difficult to see through superimposed cast material (Fig. 31-28). Closed treatment is more difficult if the medial side is also fractured. If the fracture of the medial malleolus is relatively distal and the medial axilla is still intact, there may be a buttress medially against which the talus can be supported in an anatomical position. However, if the medial malleolus fracture is more proximal, closed reduction often fails and the injury should be treated operatively.
Fractures associated with syndesmotic disruption (pronation-external rotation, abduction-external rotation, or Weber type C) are usually unstable and often require operative stabilization. If this is not possible, a closed reduction is obtained by gentle distraction, inversion, and adduction of the foot. The lateral collateral ligaments are usually the only intact ligaments on the distal fibula and do not provide enough control of this fragment to correct and maintain fibular length and rotation.
Isolated fractures of medial malleolus are uncommon, and the possibility of an undisplaced lateral injury should be considered. Isolated fractures are treated closed if they are undisplaced, involved the distal portion of the malleolus, or can be anatomically reduced by manipulation.
Maintenance of Reduction
The initial method of immobilization is dependent on the amount of swelling and the condition of the soft tissues. A soft, bulky, Jones-type dressing with supplemental plaster splints is more tolerant of swelling and usually provides adequate protection during the first few days after injury.
A long-leg cast is used for fractures that are unstable in rotation.76 Three-point fixation and careful molding is essential. Immobilization of the ankle in equinus should be avoided. Radiographic follow-up at frequent intervals is necessary to detect and correct loss of reduction before fracture healing. The long-leg cast is usually maintained for 4 to 6 weeks, and then a short-leg cast or fracture brace is used. Weight bearing should be delayed until there is early evidence of healing.
Stable or undisplaced ankle injuries may be managed in a short-leg cast or functional fracture brace for 4 to 6 weeks. Weight bearing is usually possible after the initial symptoms subside. The injured ankle is initially splinted and then placed in a cast or brace when swelling and symptoms decrease, usually within 3 to 5 days.
Authors' Preferred Method of Management
The fracture is reduced, if necessary, and placed in a Jones dressing with plaster splint reinforcement until the swelling begins to resolve. In the unstable injury in which anatomical restoration of the ankle joint has been achieved and operative treatment is not planned, we use a long-leg cast for up to 6 weeks, followed by a fracture brace. The patient is examined radiographically each week for the first month, so that any loss of reduction can be identified and corrected.
Stable fractures are treated with a walking cast, fracture brace, or walking boot with protected weight bearing, which is advanced as comfort allows and fracture healing progresses. The use of a fracture brace is combined with a rehabilitation program until functional return is complete.
Operative Treatment
The goals of operative treatment are to obtain an anatomical reduction that is maintained by stable fixation, resulting in a healed fracture and recovery of normal function. Operative treatment is recommended for failure of closed reduction; when closed reduction requires forced, abnormal positioning of the foot, such as forced plantarflexion and inversion; for displaced or unstable fractures of either or both malleoli that result in displacement of the talus or widening of the mortise greater than 1 to 2 mm; and in many open fractures.159,170,234,236,279,374,412 The current trend is toward recommending open reduction and internal fixation for any displaced fracture that involves the articular surface. However, each patient must be individualized and the presence of systemic disease, such as diabetes mellitus, physiologic age, activity level, and particularly osteoporosis, must be evaluated before recommending operative treatment.
General Principles159
Preoperative planning is based on evaluation of both the patient and good x-rays of the ankle. Anteroposterior, lateral, and mortise views and, in some injury patterns, an x-ray of the entire lower leg, are needed. A mortise view of the contralateral ankle may also be useful as a template in difficult fractures. The surgical procedure is carried out as soon as possible but is dependent on evaluation of the entire patient, the condition of the soft tissues, and the amount of swelling present. Initially, the ankle should be gently reduced and immobilized in a padded splint to prevent further soft-tissue injury and decrease swelling. Application of ice packs, elevation of the extremity, and compression are used to reduce swelling until operative treatment can be safely performed. Ankle swelling may peak in 1 to 7 days, and operative treatment is best done before the period of maximal swelling or after the initial swelling has resolved. Occasionally, a closed fracture with severe soft-tissue injury or swelling may need to be reduced and temporarily stabilized with traction on a elevated frame or external fixation to allow management of the soft-tissue injuries before definitive fixation. No adverse effect has been noted from a delay in surgery, provided that an anatomical reduction is eventually obtained. However, with time the fracture may become more difficult to reduce and the fixation less secure.126
The supine position and a tourniquet are generally used. The ipsilateral buttock can be raised on a sandbag or the table rotated to improve the exposure of the lateral side. The patient may be positioned prone or lateral if an approach to the posterior aspect of the ankle is needed. For most closed fractures, a firstgeneration cephalosporin is given before inflation of the tourniquet and continued for 24 to 48 hours after surgery, although the efficacy of antibiotics in clean limited orthopaedic procedures is not clear.297
Longitudinal incisions are used and should be long enough to provide adequate exposure and allow gentle retraction without undue tension on the skin. Incisions directly over bony prominences and undermining of the skin should be avoided. In most instances, the incisions can extend directly to the periosteum of the bone, resulting in full-thickness skin flaps. The skin edges should be handled gently; excessive pressure from forceps and self-retaining retractors may damage the skin. Periosteum from the edges of the fracture is gently elevated for 1 to 2 mm to enable accurate reduction. The fracture site can be opened by gentle distraction, re-creating the mechanism of injury, and organized hematoma and interposed soft tissue are removed from the fracture surfaces with irrigation or a small probe. Articular surfaces that are visible through the fracture site should be inspected for articular damage. The joint is irrigated, and any loose fragments are removed. A direct or indirect reduction is done carefully without forceful twisting of the ankle to minimize further soft-tissue injury. The reduction is held with a clamp or provisionally stabilized with K-wires before insertion of the selected internal fixation. Each of the fractures that require fixation should be exposed, reduced, and provisionally stabilized before proceeding with definitive fixation, because fixation of one malleolus may occasionally make reduction of the remaining fracture or fractures difficult. After internal fixation, the ankle is moved through a full range of motion with the fracture sites visible to check the stability of the fixation. Radiographic confirmation, especially with a good mortise view, of both the reduction and implant placement is obtained before wound closure. The leg is placed in a bulky, Jones-type dressing, incorporating a plaster splint. Mobilization of the patient and progression to weight bearing is based on the fracture pattern, stability of fixation, the philosophy of the surgeon, and the compliance of the patient.
In planning operative treatment, the entire ankle and lower leg must be considered. Although the general principles and goals of fixation are the same, the techniques of fixation used for the medial, lateral, and posterior malleolus and the syndesmosis are somewhat different and are discussed separately.159
Lateral Malleolus
The lateral malleolus is approached through an anterolateral or posterolateral incision centered over the fracture site. The incision can be placed even more anterior or posterior if exposure of the anterior or posterior tubercle is needed. In the proximal portion of the incision, the superficial peroneal nerve lies beneath the fascia and is at risk for injury. The type and configuration of the fibula fracture determines the type of fixation used.
Avulsion fractures (Weber type A) of the distal fibula may need operative treatment if displaced or associated with a medial malleolus fracture. The fracture is reduced, held with a reduction forceps, and stabilized by either a tension band technique or a lag screw. Technically, a true tension band is not possible because only static compression is obtained, but the technique is similar. Two parallel K-wires (0.045 inch) are inserted at the distal end of the fibula and engage the proximal medial cortex above the fracture site. A 20-gauge wire is then passed through a transverse drill hole above the fracture site and placed in a figure-of-eight fashion around the bent tips of the protruding K-wires (Fig. 31-29). Alternatively, a 4.0-mm cancellous screw or malleolar screw is placed so as to gain purchase in the proximal medial cortex of the fibula above the fracture site (Fig. 31-30). The screw head of the malleolar screw may be somewhat prominent, and the newer cannulated self-drilling, self-tapping screws greatly simplify the procedure with less exposure and are less prominent. Care should be taken that the distal fragment does not rotate or displace as the screw is tightened or that the distal fragment is not split by excessive tightening. The tension band technique may be somewhat simpler to use, especially with a small fragment or in osteoporotic bone.
The most common fracture of the fibula is caused by external rotation, resulting in an oblique fracture at the level of syndesmosis (Weber type B). After reduction, the fracture is fixed with one or two lag screws placed perpendicular to the line of the fracture. A 2.7-mm or 3.5-mm cortical screw is used, depending on the size of the fibula. An oblique fracture that is longer than two times the diameter of the bone can be fixed with lag screws alone (Fig. 31-31). More commonly, a plate is used to neutralize the rotational and axial forces on the fibula (Fig. 31-32).

Fig. 31-32 C-D La 6 luni
The one-third tubular plate conforms to the curvature of the fibula and has a lower profile than the thicker compression plates. The distal fibula also has a lateral bow, which should be restored as part of an anatomical reduction.99 The plate must be contoured to accommodate this bow to prevent medial displacement of the fracture or excessive compression of the mortise. The plate is fixed with 3.5-mm cortical screws. It is usually possible to place two or three screws distal to the fracture and three screws proximal to the fracture. The distal screws should engage the medial cortex of the fibula but not protrude into the fibulotalar joint.
The fibular plate can also be positioned posteriorly as an antiglide plate to resist proximal migration and rotation of the distal fragment.55 This is particularly helpful in elderly patients with osteopenic bone where a lateral neutralizing plate may contribute to wound healing problems and fixation may be tenuous.405 In this case, a more posterior approach to the fibula is required. The peroneal tendons are retracted, and some of the proximal retinaculum may need to be released to expose the distal fibula. The fracture is reduced, and the plate is contoured to the posterior fibula. Screws are placed in the proximal fragment, and a lag screw is placed from posterior to anterior through the plate across the fracture site. More distal screws are not necessary but may be used at the surgeon's discretion.
Fractures above the syndesmosis (Weber type C) result from external rotation or abduction forces that also disrupt the syndesmosis and are usually associated with an injury to the medial side. Transverse fibula fractures are reduced and fixed with a one-third tubular plate applied to provide compression at the fracture site. A screw is eccentrically positioned on each side of the fracture so that compression occurs when these screws are tightened. Alternatively, the plate can be fixed to one side of the fracture and then placed under tension using a clamp or tensioning device. Oblique fractures may be fixed with a lag screw or screws and a neutralization plate. If comminution is present, the size, number, and position of butterfly fragments determines whether these fragments are reduced and fixed with lag screws or reduced using an indirect reduction technique and then spanned with a plate using screw fixation proximal and distal to the fracture site. Regardless of the fixation, the soft-tissue attachments of the bony fragments must be preserved (Fig. 31-33). The most important single step is to restore the length of the fibula. Anatomical reduction of the fibula (and medial malleolus if fractured) will usually restore the mortise, and additional fixation of the syndesmosis may not be needed, especially if the fibular fracture is within 3 to 4 cm of the joint.27
Fractures of the proximal fibula (Maisonneuve type), especially those around the neck of the fibula, may not need to be internally fixed. Exposure of the proximal fibula carries an increased risk of injury to the peroneal nerve, which is fairly intolerant of traction. If the normal relationship of the fibula to the ankle and talus (length, rotation, and position in the tibial groove) can be restored and maintained, the proximal fibula fracture can be left to heal without specific treatment. The length and rotation of the fibula is restored by indirect reduction (as described below for comminuted fractures). Associated avulsion fractures of the anterior or posterior tubercle should be internally fixed. If the syndesmosis is still unstable, it should be reduced and held with one or two syndesmotic screws as described below (see Fig. 31-43).159
Comminuted fractures of the fibula are often high-energy injuries resulting from direct lateral trauma or vertical loading.230 There may be an associated impaction fracture of the lateral tibial plafond, metaphysis of the tibia (pilon fracture), and medial malleolus.83,258 In these fractures it is important to have an x-ray of the opposite and, it is hoped, uninjured ankle as a template. The comminution alters the normal landmarks and makes it difficult to judge rotation and length. The medial side, if fractured, is stabilized first to guide the reduction of the fibula. Anatomical restoration of all of the comminuted fragments may be neither necessary nor possible. Indirect reduction techniques, which preserve soft-tissue attachments to the fragments, are used to restore the correct length and rotation of the fibula.64 One such technique is to grasp the distal fibula with a pointed reduction clamp and, under fluoroscopic control, reduce the fibula using the position of the distal fibula relative to the lateral facet of the talus as a guide. A provisional K-wire is placed from the fibula into the talus or into the tibia. X-rays are obtained to confirm reduction and are compared with the 'template' x-rays of the opposite side. A plate is contoured to span the area of comminution. Alternatively, a plate is fixed first to the distal fragment. This plate is then pushed distally, distracting the fracture site, using the tension on the attached soft tissues to realign the comminuted fragments. The plate is provisionally stabilized by placing a screw in the proximal and distal fragments, and intraoperative radiographs are taken. The plate is then secured when complete fibula length has been restored as confirmed on x-ray.
The position of the plate is dependent on the level of the fracture, the condition of the overlying soft tissues, and the extent of the comminution. A plate along the posterior surface of the fibula allows a thicker, stronger plate to be used with less risk to the overlying soft tissues, but it may irritate the peroneal tendons. In this position, the distal screws may obtain a better purchase, because they are directed from posterior to anterior in the thicker part of the distal fibula and can securely engage two cortices without risk of joint penetration.256
Comminuted or segmental fractures may require other special fixation techniques or fixation over a longer length than is possible with the standard (eight-hole) one-third tubular plate. Two tubular plates can be overlapped or 'stacked' by two or more holes if there is a segment of intact fibula (Fig. 31-34), or a 3.5-mm reconstruction plate (available up to 18 holes) can be used. If comminution extends into the distal part of the fibula, a tubular plate can be modified into a 'hook plate' to provide an additional point of fixation.55
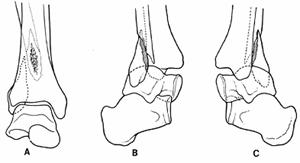 Other, less common
variations in the injury to the fibula have been described. Fixed displacement
of the fibula behind the tibia was first reported by Bosworth37 and then by
others (Fig. 31-35).165 Clinically, the
foot is in severe external rotation. Anterior dislocation of the fibula has
also been reported.341 Although it may be possible to
correct the position of the fibula with closed manipulation, the pattern of
associated injuries, including those to the fibula, often requires operative
treatment.
Other, less common
variations in the injury to the fibula have been described. Fixed displacement
of the fibula behind the tibia was first reported by Bosworth37 and then by
others (Fig. 31-35).165 Clinically, the
foot is in severe external rotation. Anterior dislocation of the fibula has
also been reported.341 Although it may be possible to
correct the position of the fibula with closed manipulation, the pattern of
associated injuries, including those to the fibula, often requires operative
treatment.
Fig. 31-35
Intramedullary fixation of the fibula has been achieved with a Steinmann or Rush pin.403 The intramedullary canal may be small and difficult to locate, and the intramedullary pin must accommodate the valgus angulation of the distal fibula. This type of fixation offers much less predictable control of rotational and axial forces. Displacement and shortening can occur even when the intramedullary device is supplemented by cerclage wires (Fig. 31-36).
Intramedullary nails designed specifically for the distal fibula provide better fixation and have been reported to give results comparable to plate fixation; however, these techniques have not gained widespread use.267
Nonrigid techniques of fixation
using combinations of cerclage wires, staples, and sutures have been used
extensively in many parts of
Biodegradable screws and rods have been reported to give results comparable to traditional stainless-steel implants.29,57,102,134,305 The primary advantage of these implants is that a second operation for removal of painful hardware would not be necessary and the elimination of long-term stress shielding. Possible disadvantages include the development of sterile sinuses as the implant degrades. Böstman and associates29 reported 8% of 62 patients with displaced ankle fractures managed with polyglycolide rods developed an accumulation of sterile fluid, and Partio and colleagues305 found sinus formation in 7% of 152 patients with ankle fractures stabilized by the same material. Frkjaer and Mller do not recommend the use of polyglycolide rods, owing to the complication rate in their prospective study of 25 displaced ankle fractures. Bucholz and associates57 found that polylactide screws were a safe and effective alternative to stainless-steel screws for fixation of displaced medial malleolar fractures in a series of 155 patients. Late spontaneous drainage was not noted in any patient in the study group. However, it was their clinical impression that polylactide screws do not provide the same amount of compression as metal screws.57
Medial Malleolus
The treatment of deltoid ligament injuries in association with the fractures of the lateral malleolus has in the past been controversial. Both operative44,80,109, 196,414,415 and nonoperative treatment of the deltoid ligament injury has been recommended.15,18,98,99,151,159, 180,250,410 Because the talus follows the fibula when the deltoid is ruptured, anatomical restoration of the fibula usually restores the talus to its normal position. It is now generally believed that an anatomical reduction of the fibula and talus restores the medial anatomy and will allow the medial ligamentous structures to heal without the need for operative repair. If, however, the medial clear space is widened by more than 2 mm after reduction of the fibula, or the reduction of the fibula is blocked, then the medial side should be explored. Interposed soft tissue, such as fibers of the ruptured deltoid ligament, may need to be removed. The posterior tibial tendon can also become trapped in the joint, but this is uncommon.84,388 Rupture of the posterior tibial tendon has also been reported.339,355,417 Repair of the deep deltoid ligament may be difficult because of its transverse position under the malleolus, short length, and the difficulty in getting sutures to hold in the remnants of a ruptured ligament. A medial arthrotomy may still be indicated if loose fragments are present in the joint, even though the ligament is not repaired.
Avulsion fractures of the medial malleolus can often be treated closed if they are isolated, minimally displaced, and involve the distal portion of the malleolus. If there is displacement or an associated lateral injury, these fractures are reduced and fixed with either a tension band technique (to achieve static compression) or cancellous screws.159 On the medial side, the tension band figure-of-eight wire can be anchored proximally through an anterior to posterior drill hole in the metaphysis or by wrapping the wire around the head of a screw (with washer) placed slightly oblique in the metaphysis (Fig. 31-37).159
A fracture above the deltoid attachment is reduced and provisionally stabilized with K-wires or 2.0-mm drill bits placed perpendicular to the fracture. Each wire or drill bit is then removed and replaced with a 4.0-mm cancellous screw. Alternatively, small cannulated cancellous screws can be placed over each K-wire. Two points of fixation are needed to control rotation of the medial malleolar fragment, and either two screws or a combination of a screw and a K-wire are used (Fig. 31-38). The screw threads should gain purchase only in the distal metaphysis 2 to 4 cm above the joint, where the densest cancellous bone is present. It is not necessary to engage the opposite cortex unless osteoporosis is present. The malleolar screw, originally designed for use in the medial malleolus, has been replaced by the use of smaller implants that have a lower head profile and are less prone to fracture the malleolar fragment.
If the medial malleolus is also fractured in the coronal plane or splits during attempts at fixation, screw purchase may be difficult. A small, one-quarter tubular plate can be contoured to run along the anterior, distal, and posterior edges of the malleolus and is used as a washer to support the placement of screws. Alternatively, the individual fragments can be reduced and each fragment fixed with a single K-wire. A series of figure-of-eight wires can then be placed around these K-wires to secure the fragments.
Fractures can result in comminution or impaction of the tibial articular surface, especially those that originate at or involve the superior medial corner of the mortise (adduction type). At the time of reduction, both the articular surface and the edges of the fracture should be inspected so that impaction of the articular surface can be recognized and elevated. A small bone graft may be needed and can be obtained from the adjacent distal tibia.
Vertical fractures of the medial malleolus are fixed with cancellous screws placed perpendicular to the fracture site. Because this fracture pattern is subject to vertical shear forces, it is important to buttress the fracture by placing a screw with a washer at the proximal apex of the fracture or to use a small tubular plate or T-plate as a buttress (Fig. 31-39).
Posterior Malleolus
There continue to be differences of opinion as to the indications for operative treatment of the posterior fragment. Open reduction and internal fixation has generally been recommended when more than 25% of the posterior articular surface is involved or the fracture is displaced more than 2 mm. These indications are based largely on several retrospective clinical studies, which found an increased incidence of unsatisfactory results, usually due to posterior subluxation of the talus, when the posterior fragment exceeded 25% of the articular surface.262,264,265,284 Harper and Hardin 153 have pointed out that these results may be due, in part, to less than anatomical reduction of the associated medial and lateral fractures, which were often treated nonoperatively. They found that an anatomical reduction and fixation of the fibula reduces and stabilizes both the talus and the posterior fragment; in patients with involvement of 25% to 45% of the articular surface there was no difference between the results obtained with or without internal fixation of the posterior fragment.152,153 Other reports of operative treatment have continued to support the recommendations of internal fixation for fractures involving more than 25% of the articular surface.158,159,234,259,374,403
The lateral x-ray may be unreliable in assessing the size of the posterior fragment because the fracture plane is usually oblique to this view. Oblique films or occasionally a CT scan may be helpful. Ferries and associates123 evaluated 25 patients using both conventional radiography and CT and found that plain radiographs erred in most cases by overrating the size of the fragment and were unreliable in assessing the posterior fragment size.
As the fibula is reduced, the posterior tibiofibular ligament often pulls the posterior fragment into a reduced position. Dorsiflexion of the foot may assist in reduction by a ligamentotaxis effect from the posterior capsule. The decision to fix the posterior fragment is based on the size of the fragment, the amount of residual displacement after reduction of the fibula, the perceived functional demands of the patient, and the experience of the physician. Fixation of a fragment, regardless of its size, may be indicated to stabilize the syndesmosis, if there is persistent posterior subluxation of the talus after reduction of the medial and lateral fractures or if the fracture involves the tibial groove and fragments prevent reduction of the fibula.
The posterior malleolus may be stabilized by either a direct approach to the fracture with placement of screws from posterior to anterior or by indirectly reducing the fracture and placing screws from anterior to posterior. For a direct approach to the posterolateral malleolus, the fibula should first be reduced. The interval between the peroneal tendons and the flexor hallucis longus muscle allows exposure of the posterior tibia. The articular surface cannot be seen after the fracture is reduced, and the external edges of the fracture are used as a guide to anatomical reduction. In some fractures this may not be reliable, owing to comminution along the edges of the avulsed tubercle. Provisional stabilization with K-wires and radiographic confirmation of reduction should be obtained before screw placement. The fracture is fixed with one or two cancellous screws placed from posterior to anterior (Fig. 31-40). Fractures involving the posterior malleolus can also be approached through an extended posteromedial approach, with dissection in front or behind the medial neurovascular bundle and flexor hallucis muscle, depending on the location of the fracture.
Two problems can be encountered when placing the screws from the anterior aspect of the tibia into the posterior fragment: (1) the fracture can be displaced by the passage of a Kirschner wire, drill bit, or screw, and (2) it may be difficult to achieve a lag screw effect (no screw threads with purchase on both sides of the fracture) in a small posterior fragment. For anterior to posterior fixation of a small fragment, a cortical screw can be placed as a lag screw or a 4.0-mm cancellous screw, with some of the threads cut from the end of a longer-than-measured screw, can be used.159,259 Anterior to posterior fixation is easiest when all three malleoli are fractured. The fibula is reduced and held with a clamp, and the joint is inspected through the medial malleolus fracture site. With gentle distal traction the articular surface of the distal tibia is easily seen, and exact reduction of the posterior fragment can be confirmed. This fragment is held with a nerve hook or meniscus probe placed through the joint, or a blunt instrument such as the tip of a screwdriver placed directly against the posterior fragment through the fibular incision. Lag screws are placed through a separate anterior incision (see Fig. 31-32C and D). Small cannulated screws placed over the provisional K-wires can be used with either the direct posterior or the indirect anterior approach.
Isolated posterior malleolus fractures are uncommon and result from vertical loading or anterior displacement of tibia on a planted foot. Involvement of more than 25% of the articular surface, posterior instability, and subluxation of the talus are indications for operative treatment.
Anterior Malleolus
Isolated fractures of the anterior margin of the tibia are uncommon. They most often result from vertical loading or from posterior displacement of the tibia on a planted foot. Occasionally, an avulsion fracture of the anterior tibial tubercle will involve a large portion of the anterior tibia (see Fig. 31-27). Indications for operative treatment are the same as for the posterior malleolus. Lag screws alone are usually sufficient fixation, but a buttress screw or plate may be needed if the fragment extends into the distal shaft of the tibia.
The pilon fracture is among the most challenging problems faced by the orthopaedic surgeon. Historically, the term pilon was first used by Destot in 1911.100 He compared this explosive injury of the talus impacting against the tibia to that of a hammer striking a nail. Bonnin,33 in 1950, emphasized that this fracture involved the tibial plafond of the ankle joint. As more experience with this fracture has been gained, the large compressive forces with the resulting crush injury and the significant disruption of the articular surface have been recognized.14,33,44,47,88,196,215,220, 244,257,332,384
This fracture with the soft-tissue injuries associated with it, has been among the most difficult to treat. With the advent of greater numbers of motor vehicular accidents, falls from heights, and penetrating trauma, the numbers of these injuries have increased, because they are associated with high-energy insults. The soft tissue may be degloved, and a large amount of crush necrosis is associated with this fracture. These high-energy injuries are also associated with severe bone comminution and, unfortunately, may be only one fracture of many injuries in a multitrauma patient. Fortunately, most large series still report only 7% to 10% incidence of tibial fractures as pilon fractures.40
Mechanism of Injury
The primary component of force is vertically directed through the talus into the distal tibia. The severity of bone, cartilage, and soft-tissue damage is directly proportional to the amount of energy involved in the traumatic event. Thus, sporting injuries such as skiing accidents tend to have a better prognosis than higher energy injuries such as motor vehicle accidents or falls from great heights.
The compressive nature of the injury also results in significant articular damage to the talus and tibial plafond. The initial severity of damage may be among the most important factors in predicting long-term outcome. In addition, the condition of the fragile soft tissues will greatly affect the ability of the injury to heal.
The position of the foot on impact in combination with any torsion, bending, or shearing forces will affect the configuration of the fracture pattern.243 In plantarflexion, the compressive forces are directed posteriorly. This causes an increased tendency for larger posterior lip fragments and more posterior comminution. Conversely, in the dorsiflexed foot, the compressive forces are directed primarily in an anterior direction, leading to greater anterior lip fragments or comminution. Angular and rotational forces will lead to greater metaphyseal extension of fractures with varying degrees of comminution medially or laterally. Clearly, the superimposition of all these forces can lead to fracture patterns that defy any classification.
Classification
Early attempts at a classification scheme met with difficulty owing to the complex nature of the injury. Gay and Evard139 made an early attempt at classification in the European literature. Lauge-Hansen added a fifth fracture type to his ankle classification to account for pilon fractures.219 Rüedi and Allgöwer,330 however, have proposed a classification scheme that is simple and clinically relevant (Fig. 31-41). Type I fractures are cleavage fractures of the articular surface with minimal displacement of the intra-articular fracture fragments. Type II fractures involve significant displacement of the intra-articular fractures without comminution but moderate intra-articular incongruity. Type III fractures are similar to type II fractures but have significant comminution with impaction of the distal tibia and gross incongruity of the articular surface. Maale and Seligson243 added to this classification a category for spiral fractures of the distal tibia in which the distal extension enters and disrupts the joint's weight-bearing surface.
Mast and Spiegel257 also described a classification system with prognostic significance. In this system, type I fractures are similar to malleolar fractures as described by Lauge-Hansen with a large posterior plafond fragment. Type II fractures are spiral extension fractures as described by Maale and Seligson. Type III fractures are central compression fractures from talar impaction into the tibial plafond. These type III fractures are further subdivided by the Rüedi-Allgöwer classification. Prognosis worsens from type I to type IIIC.
Fig. 31-41
Another popular classification scheme is that proposed by the AO group. Pilon fractures are divided into type A: extra-articular fracture; type B: partial articular fracture involvement with a portion of the tibial shaft intact; and type C: completely articular fracture with no continuity between the articular surface and tibial shaft. Within each type, the fractures are further divided by the amount of fracture gap, joint depression, and degree of comminution.
Signs and Symptoms
Meticulous examination of the skin, soft tissues, and neurovascular structures, including pulses, should be performed. The tibia is mostly subcutaneous in this area; fracture displacement or excess pressure on the skin may convert a closed fracture into an open one. Swelling is often rapid and massive, and the fracture should be reduced and splinted as soon as the examination is complete. Subsequent edema, fracture blisters, and skin necrosis from the original injury may still convert closed fractures to open injuries, and continued soft-tissue monitoring is important. In addition, since many patients are victims of multitrauma, associated injuries are common and must be treated appropriately.
The standard three views of the ankle and a 45° external rotation view to delineate the anteromedial and posterolateral surfaces of the tibia should obtained. Computed tomography with coronal and sagittal reconstructions or conventional tomography may be considered to better evaluate the fracture pattern. A radiograph of the normal contralateral ankle may be used as a template guide for preoperative planning. Treatment options are based on many factors, including the age and functional status of the patient, the degree of injury to the bone, soft tissues, and cartilage, the degree of osteoporosis and comminution, the 'personality of the fracture,'258 and the capabilities of the surgeon.
Treatment
Nonoperative Treatment
Closed Reduction and Casting. Accurate reduction of the intra-articular fragments is unlikely with simple manipulation. Casting prevents observation of swelling and the skin, and loss of reduction is common. This treatment is indicated primarily for undisplaced fractures or in debilitated patients.
Traction
Distraction of the fracture using calcaneal traction may result in satisfactory alignment if the central portion of the articular surface is not crushed and impacted. Traction allows direct access to and elevation of the leg and may be combined with early motion and rehabilitation of the joint. Management by traction does require the patient to remain in bed until early evidence of union has occurred, usually a minimum of 6 weeks.
Traction may also be used initially in those fractures in which operative intervention is planned but must be delayed because of the status of the soft tissues. In these cases the ligamentotaxis effect of calcaneal traction can produce a provisional reduction and maintain length until surgical intervention can be accomplished safely.
Operative Treatment
Open Reduction and Internal Fixation. The goals of surgical treatment as outlined by Rüedi and Allgöwer330 are as follows:
Maintenance of length and stability of the fibula
Restoration of tibial joint articular surface
Restoration of bone defect
Buttressing of the medial tibia
In treating tibial pilon fractures there are many surgical options. However, the treatment of the fracture must always be tempered by the fragility of the soft tissues, and management of each fracture case will need to be individualized depending on the status of the soft tissue. The emphasis on anatomical reduction of the tibial plafond with restoration of the joint surface is generally recognized as a primary goal.14,33,44, 47,88,196,215,220,244,257,332,371,384 It is also helpful to estimate the degree of osteoporosis and comminution since poor bone quality will hamper surgical stabilization.47
A posterolateral incision is used for fibular fixation. An anteromedial incision just 1 cm medial to the anterior tibial tendon curved toward the medial malleolus is used to fix the tibial plafond and tibial metaphysis.280 Care must be used not to undermine the soft tissues and deglove the anterior tendons. This is true especially because paratenon will accept both free flap and soft-tissue grafts but exposed tendon will not. Care must also be used to maintain an 8-cm skin bridge to avoid anterior skin necrosis and wound breakdown, especially over the medial incision.
The four basic principles as described by Rüedi108 are followed. The initial step is to reduce and stabilize the fibula. This step restores length at the lateral articular surface syndesmosis and provides a reference point for the remainder of the reconstruction. Indirect reduction techniques or use of a femoral distractor are helpful in this phase. The articular surface of the distal tibia is then anatomically restored and provisionally stabilized with multiple K-wires. Radiographic and visual confirmation of the articular reduction should be obtained.
A variety of implants are available to stabilize the distal tibia, but the selection is dependent on the fracture configuration. Lag screws are used to compress the fracture fragments. A buttress plate is then used medially to prevent collapse. The final step involves the use of cancellous bone graft to repair the metaphyseal defect. Care must be taken to avoid devascularization of the anterior tibia and avoid a 'dead bone sandwich.'
Splinting in a Jones-type dressing with supplemental plaster, application of ice packs, and elevation of the extremity are used in the immediate postoperative period. Motion exercises are initiated as soon as tolerated by the patient, but unprotected weight bearing is delayed until the fractures have united, usually at 3 to 4 months postoperatively.
External Fixation
In patients with significant soft-tissue compromise or an open fracture, the external fixator may be used as an initial portable traction device. A reduction is obtained through distraction and ligamentotaxis. The external fixator may be used to treat the fracture until the soft tissues will allow operative treatment. It may also be used as the definitive treatment if an adequate reduction is obtained or further operative treatment becomes contraindicated.336
The external fixator has also been used as a medial buttress30 in combination with limited internal fixation. In this situation, the external fixator takes the place of the medial buttress plate but decreases the need for a large amount of soft-tissue dissection. The principles for open reduction and external fixation are used with fibular reduction and restoration of length performed first. The tibial joint surface may then be reduced as anatomically as possible and fixed with screws. An external fixator is used in place of the medial buttress plate. This external fixator may be replaced by a plate at a later date or left as the definitive form of treatment. Any metaphyseal defect may be grafted at the time of initial surgery. It may also be done later, especially, if the external fixator is replaced by a plate.
A variation of this theme using hybrid fixators or small pin circular fixators has become popular.282,364,378 The reduction maneuver is enhanced using the small pins with or without olives to restore the joint surface and maintain bony stability. This technique is especially helpful when open wounds contraindicate the use of any internal fixation device of any kind. Whenever an external fixator is used, special consideration of a calcaneal pin for distraction of the tibiotalar joint should be made. In patients in whom motion of the ankle is contraindicated, the joint may be distracted and maintained this way by a calcaneal pin. This may aid in decreasing stiffness in this joint.31
Authors' Preferred Method of Treatment
We prefer to individualize the bony treatment of pilon fractures depending on the condition of soft tissues, the severity of the fracture, and the timing of initial presentation for treatment. All patients who present within 12 hours of injury are thoroughly examined and considered for surgery. If the soft tissues are compromised but closed, we often place patients in calcaneal traction, hospitalize them with their leg on an elevated frame in a plaster splint, and return them to surgery when their soft tissues allow. In extensive open fractures, an external fixator is used after the initial debridement in a similar procedure as outlined earlier. We have waited up to 3 weeks for adequate return of skin folds, decreased swelling, and healing of fracture blisters. Generally we return the patient to surgery within 7 to 10 days.
After the initial debridement of any soft-tissue wounds has been performed, we proceed to the fibula. We restore the fibular fracture anatomically with a dynamic compression plate or a one-third semitubular plate in those fractures with minimal comminution. This plate is placed posteriorly along the fibula to maintain as large an anterior soft-tissue bridge as possible. Generally, the soft tissues are least compromised posteriorly. The stable fixation of the fibula allows the surgeon to bring the remaining soft tissues out to length and gives a guide to the remaining fracture treatment (Fig. 31-42). If the soft tissues allow, we proceed to fixation of the tibial articular surface. Reduction is obtained with K-wires and elevation of articular fragments with periosteal elevators. This is often performed percutaneously with fluoroscopic visualization or through any open medial wound. A lag screw from posteromedial is directed laterally to buttress the articular reduction and reduce any posterior lip fragment. If a large articular defect is present, this screw may also span the defect to maintain the medial-to-lateral articular width. Loose bone fragments that cannot be stably interlocked into the joint reduction are removed. Attempts should be made to maintain any large fragment of bone with articular cartilage. Bone graft is used to span any articular defect. The medial malleolus is reduced and fixed with a lag screw or tension band technique. The metaphysis is finally reduced and fixed with a T-plate or cloverleaf plate. Bone grafting of the metaphyseal defect is also done if possible. It is important to minimize soft-tissue stripping and devascularization of the bone when placing the medial buttress plate. As the severity of the fracture and soft-tissue injury increases, we advocate the use of a medial external fixator and limited internal fixation. We will also stage our operative steps and in severe fractures may only stabilize the fracture with a fibular plate, several percutaneous screws, or K-wires to align the tibial articular joint surface and place an external fixator medially. Further manipulation of the articular joint surface and tibial metaphysis and grafting of bone defects may be done in sequential fashion at later operative sessions. We distract the tibiotalar joint when inadequate restoration of the joint surface or a large articular defect is present, thus minimizing the risks of a calcaneal pin when possible.
Whenever an external fixator is used, special consideration of a calcaneal pin for distraction for the tibiotalar joint should be made. In patients in whom motion of the ankle is contraindicated, the distraction maintained by the calcaneal pin may aid in avoiding a stiff joint.31
Complications
Early complications commonly reflect the status of the soft-tissue injury, as well as the handling of tissues at surgery. Hematomas, skin slough, and necrosis of soft-tissue bridges and flaps all affect wound healing. Eventual loss of soft-tissue coverage may compound problems with infections such as osteomyelitis, while compromising fracture healing as well.111,160,226,263 Meticulous soft-tissue management to avoid stripping and gentle handling of tissues and avoiding wound closure under tension will greatly enhance the viability of wound healing. The use of secondary skin closure when significant loss or devascularization of soft tissues has occurred, of muscle flaps, or of free flaps may need to be considered early in the course of management.111,226,263 Open injuries, crush necrosis, and degloving injuries contribute to long-term soft-tissue necrosis, infection, nonunion, or delayed union.111,226,263
Later complications include osteomyelitis, delayed union, malunion, and nonunion of the fracture. Although nonunion rates have decreased with emphasis on soft-tissue management, bone grafting of defects, and appropriate fixation techniques, it is not uncommon to encounter problems with delayed unions.160,263 Malunions are common especially with nonanatomical fracture reduction or loss of the medial metaphysis with inadequate buttressing techniques.160,263,378 Osteotomies to correct malalignment may be performed at a later date once union has been obtained, but initial maintenance of the medial buttress during healing of the fracture will minimize this problem.263,378
Traumatic arthritis is common when significant articular damage is present. Despite attempts at anatomical articular reconstruction, the severity of damage to the articular cartilage itself should not be underestimated with problems of painful degenerative traumatic arthritis as a sequela. Arthrodesis has generally been accepted as a treatment alternative to this problem and may also be used judiciously to address malalignment issues at the same time.243
Stabilization of the disrupted syndesmosis may be achieved by repairing ruptured ligaments; by fixing associated fractures of the fibula, avulsed tubercles, and medial malleolus; or by placing a screw between the tibia and fibula to hold the syndesmosis in position until some degree of syndesmotic ligament healing can occur. The frequency with which syndesmotic fixation is used has decreased significantly in recent years. Early reports describe the use of syndesmotic screws in 40% of Weber type B fractures and up to 80% of Weber type C fractures.60,147,234,259 More recent clinical and experimental studies have shown that anatomical reduction of the fibula, especially if the fracture is within 4 cm of the joint, usually reduces the talus in the mortise and restores stability to the syndesmosis.27,147,325 Fixation of a fractured medial malleolus also enhances stability by restoring function of the deep deltoid ligament. Syndesmotic fixation is now recommended only when there is medial ligamentous injury, syndesmotic disruption, and talar shift without a fracture of the fibula (tibiofibular diastasis); when the treatment of a high fibular fracture (Maisonneuve fracture) is directed primarily at stabilization of the syndesmosis and ankle mortise (Fig. 31-43); or when there is continued evidence of syndesmotic instability after fixation of the fibula and any avulsion fractures of the tubercles or medial malleolus (Fig. 31-44).259
The syndesmotic screw is a positioning screw that is used to hold but not compress the syndesmosis (Fig. 31-45). Because the fibula is posterior to the tibia, the syndesmotic screw must be angled from posterolateral to anteromedial to engage the tibia. The foot is placed in dorsiflexion to bring the widest portion of the talus into the mortise. Both cortices of the fibula and the lateral cortex of the tibia are drilled and tapped, and one or two cortical screws (3.5 or 4.5 mm) are used. If movement occurs, this screw will loosen in the lateral cortex of the tibia rather than break, as was common in the past when both lateral and medial cortices of the tibia were engaged.191 This screw is placed just above the level of the tibiofibular ligaments; if the screw is placed too high, the fibula may be pulled medially at the level of the screw, resulting in widening and lateral tilt of the distal end of the fibula. This screw is placed either through the fibula or through one of the holes in a fibular plate, depending on the level of injury (see Fig. 31-43 and Fig. 31-44).
The decision to use syndesmotic fixation is based on the fracture pattern and intraoperative assessment of stability. The stability of the syndesmosis can be tested by placing a hook around the fibula at the level of the syndesmosis and applying lateral traction. Lateral movement of the intact or internally fixed fibula and widening of the mortise on intraoperative x-rays are indications for a syndesmotic screw.
Patients with syndesmotic injuries are generally kept non-weight bearing for 6 to 8 weeks. Controversy exists as to whether the screws should be removed before weight bearing. The fibula moves in several planes during weight bearing, and it has been shown that the syndesmotic screw prevents the normal physiologic motion of the fibula, particularly external rotation.166,283,289 Several studies have shown that weight bearing with the syndesmotic screw in place had no adverse effects with no increased incidence of pain or syndesmotic ossification, provided a functional range of motion had been regained.99,191,289 Others have recommended that the syndesmotic screw be removed before weight bearing to restore the physiologic movement of the fibula and prevent fatigue failure of the screw.259,270,278,283 We prefer to start partial weight bearing at 6 weeks with the syndesmotic screw in place. The screw can be easily removed with the use of local anesthesia if the patient becomes symptomatic.

Fig. 31-45 Folosirea incorecta a surubului de sindesmoza. Talusul nu este redus in ciuda tentativei de fortare a fibulei medial.
POSTOPERATIVE MANAGEMENT
The management following operative treatment of ankle fractures remains controversial. One of the goals of internal fixation is to permit early mobilization of the involved joint to restore function and prevent fracture disease.94,159,240,283 Ideally, this would begin a few days after surgery with the ankle left free to move and begin protected weight bearing. Concerns about loss of fixation, protracted symptoms from overuse or unsupervised rehabilitation, and patient compliance have prompted many surgeons to immobilize the ankle until there is evidence of fracture healing. Many believe that it is easier and safer for a patient to walk in a cast or fracture brace than to remain non-weight bearing on crutches. There are many variations in postoperative treatment because of differences between what is ideal and what is practical. Compression bandages, air splints, posterior splints, fracture braces, modified casts that permit dorsiflexion, and weight-bearing and non-weight-bearing casts have all been used.349 Several studies have found no difference in outcome between patients treated with early motion versus those treated with immobilization.3,4,79,124,157,125,359 Postinjury osteopenia was seen regardless of postoperative treatment but tended to recover faster with early functional rehabilitation.124
Routine implant removal is controversial. These patients are often young, and long-term biocompatibility remains a concern. Symptomatic implants obviously should be removed. Although the literature generally supports leaving asymptomatic implants in place the final decision rests with the physician and the patient. Refracture after implant removal is uncommon. To avoid the problems of implant removal, biodegradable fixation has been used, but further refinement and experience is needed before these techniques can gain widespread use.28
Open injuries of the ankle require application of the same principles of open fracture management used elsewhere in the skeleton. This includes alignment and splinting of the fracture to prevent further injury; prompt operative treatment; careful, thorough debridement of the wound with copious irrigation; perioperative antibiotics; tetanus prophylaxis if needed; stabilization of the fracture; and delayed wound closure. Soft-tissue management of the open wound is the key to a successful result. Stabilization of the fracture fragments maximizes the ability of the soft tissues to heal and resist infection. The increased experience with internal fixation in the treatment of closed fractures has led to successful application of these techniques in open fractures.45,46,74,130,406 The goals of treating an open ankle fracture are similar to those for treating a closed fracture: anatomical reduction with complete return to normal function and prevention of infection.
Preoperative planning is essential in treating these injuries because the surgical exposure and implant placement may need to be modified by the presence and location of open wounds or damaged skin. Many of these patients have multiple injuries, and the treatment of their open ankle fracture must be coordinated with the management of the other associated injuries. A tourniquet is usually placed around the thigh but is not used unless absolutely necessary. Operative treatment can be divided into three stages: debridement, fracture stabilization, and reevaluation and wound closure.
First, the wound must be thoroughly cleansed and debrided. The open wound usually communicates with the ankle joint, and contamination can be more extensive than the external wound suggests. Wounds resulting from farm or fresh water injuries and especially those with soil contamination can be particularly troublesome. Many open wounds are transverse and may need to be extended to obtain adequate exposure. Vertical incisions at the ends of these transverse wounds, creating a Z- or L-shaped incision or occasionally a T-shaped incision, usually provide an adequate exposure for debridement and treatment of the fracture. Cruciate incisions should be avoided. The joint should be thoroughly inspected because articular and bony fragments as well as contaminated material can lodge in the recesses of the joint. If the capsule is torn, this contaminated material can also be found in the soft tissues outside the joint.
The second stage of treatment begins after cleansing of the wound and joint is complete. The instruments required for the debridement are removed, the operative team changes gowns and gloves, and the ankle is redraped. If other fractures not associated with the open wound are present and need fixation, they are now exposed. Soft tissues must be carefully protected and unnecessary stripping of the periosteum avoided. In grades I, II, and many grade III fractures, fixation can be carried out using the minimum number of implants that will achieve stable fixation. Ideally, implants and bone should be covered with soft tissue, but this is not always possible. The potential for leaving screws or a plate exposed is not a contraindication to internal fixation. Reduction and implant placement should be confirmed radiographically. The surgical incisions are then closed if possible and the traumatic wound is left open.
The third stage of treatment is reevaluation of the wound, repeat debridement if needed, and delayed closure if the wound is clean. Timing of wound closure is based on the condition of the wound and the severity of the contamination. It may be possible to close the skin directly or to use skin traction with a rubber band technique. Some wounds can be managed with dressing changes and allowed to heal by secondary intention. Occasionally, a split-thickness skin graft is required, but transposition or free flaps are usually not needed for ankle fractures.130
In open injuries with extensive comminution, such as a crush injury or pilon fracture, it may not be possible to use internal fixation. These injuries have been treated using transarticular transfixion pins placed through the calcaneus and talus and into the tibia.77 The availability of more versatile external fixation devices now makes external fixation preferable to transfixion pins. Fixator pins can be positioned proximally in the tibia and distally in either the talus or calcaneus or both and provide adequate stabilization as well as allow exposure of the wound. A pin can be placed into the metatarsal and incorporated into the external fixation frame to prevent equinus contracture of the ankle. Many different external fixators and frame configurations are available that provide a wide range of treatment options from temporary stability until soft-tissue coverage is achieved to definitive fracture management. Alternatively, a calcaneal pin with skeletal traction and elevation on a lower extremity frame, such as a Böhler-Braun frame, can be used. The traction will provide some reduction by ligamentotaxis and also allow some early movement of the joint, which may assist in the remodeling of the articular surface.
Reports on the treatment of open ankle fractures have shown that immediate internal fixation can be done with a low incidence of infection and with union rates nearly equal to that of closed fractures.46
Authors' Preferred Method of Treatment
We prefer to manage open ankle fractures by immediate wound debridement followed by reduction and internal fixation. Repeat debridement is done as often as needed, usually at 2- to 3-day intervals. Skin closure is delayed until the wound is clean.
SPECIAL TREATMENT PROBLEMS
The presence of systemic disease such as diabetes, peripheral vascular disease, metabolic bone disease, or obesity may complicate the treatment of ankle injuries. Treatment of the ankle is based on the injury pattern and evaluation of the systemic problem and its effect on the extremity. Diabetes increases the risk of infection and can lead to decreased cutaneous and deep circulation, peripheral neuropathy, osteoporosis, and delayed healing. Patients at greatest risk for operative treatment may also be difficult to treat in a cast because of advanced disease, poor skin, and porotic bone. Neuropathic changes in the ankle or foot can result from what appears to be a minor injury. Increased joint stress from a nonunion or malunion may also contribute to the development of a neuropathic joint.
Ankle fractures in elderly patients may also present difficult treatment problems.7 As population demographics change, these fractures are becoming more common, and many occur after otherwise minor injuries.17,22 The decision for closed or open treatment must be individualized, considering the physiologic age, activity level, and medical status of the patient, as well as the risks and benefits of the available treatment options. Fractures in osteoporotic bone are often comminuted and fixation may be difficult. Occasionally, in patients with severe osteopenic bone, we place a large Steinmann pin through the calcaneus and talus into the tibia to help stabilize the talus in the mortise in an effort to decrease the forces on the fixation. Although better results have been reported after operative treatment the complication rate, particularly in osteoporotic female patients, is also higher.21,239
COMPLICATIONS
Nonunion
Most nonunions involve the medial malleolus.269 These are often avulsion injuries that were initially treated closed and fail to unite because of residual displacement of the fracture, interposed soft tissue, or associated lateral instability resulting in shearing forces on the fracture from the pull of the deltoid ligament. A nonunion in the distal portion of the medial malleolus is often not symptomatic, especially if the lateral ankle is stable. Nonunions at the level of the joint may cause chronic pain, swelling, and a feeling of instability. Symptomatic nonunions have been treated with open reduction and internal fixation and sometimes with electrical stimulation.48 An exact reduction may be difficult because of resorption at the fracture site and remodeling of the fracture edges. Osteoporosis of the distal fragment may make fixation difficult. Gaps are filled with bone graft, and fixation is performed with either a tension band technique or cancellous screws.
Nonunion of the lateral or posterior malleolus is uncommon. The displaced fibular fracture usually settles into a stable position if unreduced and then heals. Nonunion after operative treatment can occur if the bone is extensively comminuted or devitalized, the reduction is incomplete, or the fixation is inadequate. Avulsion fractures of the lateral malleolus may have a fibrous type of union and are usually not symptomatic.
Malunion
Because most ankle fractures involve metaphyseal bone that usually heals, malunion is more common than nonunion. Incongruity of the articular surface and instability of the mortise due to bone or ligament malunion can alter the mechanics of the joint and lead to persistent symptoms, degenerative changes, and loss of function of the joint.49,288 Mont and associates275 reviewed the radiographs of 80 consecutive displaced ankle fractures treated operatively and found that the radiographic factors most predictive of a poor outcome were an abnormally wide medial clear space and the presence of a large posterior malleolar fragment.
Impaction fractures resulting in malunion of the articular surface of the talus or tibia are often unrecognized. The medial articular surface of the tibia may be compressed by forced adduction of talus, while the lateral articular surface and anterior margin of the tibia may be damaged by axial loading, rotational, or translational forces.83
The medial malleolus may be pulled distally by the deltoid ligament and, if not reduced, heal in this elongated position. This is infrequently symptomatic but can cause problems when associated with lateral instability, with irritation of the posterior medial tendons, or with shoe wear. Malunion can occur after internal fixation if the initial reduction was not exact or if fixation fails to maintain the reduction. Rotation can occur when only a single point of fixation is used. Unrecognized comminution can result in shortening or rotation of the medial malleolus and in failure to restore the articular surface.
The posterior malleolus often reduces as the other components of the ankle fracture are reduced. This fracture can displace superiorly after what initially appeared to be a good reduction. If the posterior fragment is important to the stability or surface area of the joint, internal fixation should be considered. Once this fracture has healed, residual displacement is difficult to correct. Because a posterior malleolus fracture of 25% to 30% of the articular surface does not usually require reduction and fixation, malunion of a fragment of this size is usually not a problem. Malunion of a larger amount of the articular surface may need to be corrected to prevent arthritis, especially if the talus subluxes into the posterior defect. A preoperative CT scan is helpful in planning the operation. A lateral approach with osteotomy and distal reflection of the fibula and use of a femoral distractor may be needed to adequately see the articular surface and correct the malunion.64
Fibular Malunion
A painful arthrosis after ankle fracture may result from (1) severe cartilage damage at the time of injury, (2) a malaligned and shortened lateral malleolus allowing the talus to shift laterally, or (3) a combination of these factors.
An arthrodesis is the treatment of choice for severe cartilage damage, while for the shortened fibula with some cartilage damage a fibular osteotomy with lengthening may relieve the pain and allow a functional recovery. Many authors support this as an acceptable procedure even at a long time after fracture and with signs of arthrosis.170 Experimentally, Ramsey and Hamilton318 and others206,408 have shown the importance of an anatomical reduction of the lateral malleolus. Any shortening of the fibula allows the talus to shift laterally, decreasing the normal contact area between the talus and the tibia. The principal indication for the fibular osteotomy that restores normal length is radiographic evidence of a shortened fibula with any shift of the talus laterally.
Preoperative Evaluation
Standard anteroposterior and lateral x-rays, with a mortise view taken with the affected and normal ankle at 20° of internal rotation and the foot at neutral, will outline the talus to be either in a valgus position, laterally displaced, or both. These sets of film will give a clear comparison, indicating if the fibula is shortened, lateralized, or externally rotated.327
Four characteristics have been described that will reveal an abnormal mortise secondary to a shortened fibula (Fig. 31-46).
The joint space will no longer be strictly symmetric but will reveal a widening on the medial side.251
The 'Shinton's line of the ankle,' which is the dense subchondral bone of the distal fibula and tibia, will be broken. Normally, there should be a general connecting arc, the spike of the fibular subchondral bone plate pointing directly to the lateral tip of the tibial subchondral bone plate.251
The normal relationship between the lateral articular surface of the talus and the medial fibula will be altered.
A fourth finding, widening of the talocrural angle, may or may not be present.96
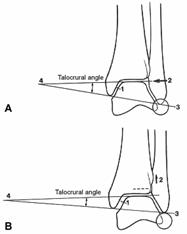
Fig. 31-46 A) Glezna normal se vizualizeaza in RI de 20 grade. 1) toate spatiile dintre tibie si talus sunt echidistante; 2) linia subcondrala (linia Shinton) de la fibula la tibia distala este neintrerupta; 3) exista o curba neintrerupta intre fibula distal si talus lateral; 4) unghiul taqlocrural este normal . B) 1) Fibula scurtata determina largirea spatiului articular medial; 2) linia subcondrala devine intrerupta prin ascensionarea fibulei; 3) curba intre fibula distal si talus lateral evidentiaza scurtarea fibulei; 4) unghiul talocrural scade.
Surgical Approach
The patient is placed in a supine position with a small sheet beneath the iliac crest on the affected side. A pneumatic tourniquet and x-ray control should be available in all cases. The entire lower leg is prepped along with the iliac crest, and a standard lateral incision is used to expose the fibula. If the fracture is recent and a pseudoarthrosis is present, the fibula may be lengthened at the original fracture line. When such is the case, the fragments are mobilized, the fracture is reduced and the fibula is positioned with a K-wire through the distal fragment into the tibia. A mortise view radiograph is then taken to check the fibular position. If the reduction is sufficient, a narrow 3.5-mm five-hole AO plate is secured to the fibula and bone graft is applied in the area. It may be necessary to approach the medial side of the joint and clean the debris from the medial malleolar-talar area.250,288
In most cases, the fracture will be healed and therefore require a fibular osteotomy, which may be accomplished in the original fibular fracture site. The saw cut is made and lengthening accomplished by the use of an AO tensioning device or the AO small external fixator (Fig. 31-47). We prefer to use the AO tensioning device. After the osteotomy is accomplished, a small five-hole 3.5-mm AO plate is secured with two screws in the distal portion of the lateral malleolus. Weber394 makes a point of the plate being applied to internally rotate the lateral malleolus, but other authors believe the problem is not an externally rotated fibula but an internally rotated proximal fibula.127 At this point, the tensioning device is applied with the hook proximally set so that the device can push the locked distal fibula distally. If movement does not occur easily, the incisura should be cleaned out surgically. An x-ray is used to check for a proper lengthening. The lengthening should be equal to that of the normal side. All of the x-ray parameters are viewed to make sure a proper correction is accomplished.
After the correction is accomplished, a small corticocancellous graft is taken either from the medial tibia or from the iliac crest and placed into the osteotomy site. The osteotomy should be opened a little wider and the graft put in place. Then the tensioning device is converted to a compression mode. When the corticocancellous graft is locked in place, the proximal three screws are placed.
A small drain is inserted, the lateral incision closed, and a posterior splint is applied. The drain is removed at 24 to 36 hours and the dorsal dressing is split, allowing the patient to dorsiflex the ankle. With the removal of skin sutures on the 10th day, a short-leg walking cast is then applied and worn for 6 to 8 weeks or until healing is consolidated.
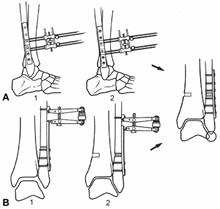
Fig. 31-47
Wound Problems
Marginal necrosis of skin edges after surgery occurs in about 3% of patients.234 Carragee and associates65 reviewed the early complications in 121 surgically treated closed ankle fractures and found that fractures with skin blisters or abrasions had more than double the overall complication rate. These problems can be decreased by avoiding surgery during the period of increased swelling; minimizing tourniquet time; careful handling of the soft tissues, especially the skin edges; gentle retraction; use of implants appropriate for the size of the fracture fragments; wound closure without tension; appropriate drainage of the wound; and avoiding constrictive postoperative dressings. Problem wounds can usually be managed with dressing changes, and most will fill in with granulation tissue and heal.
Major wound problems occur more frequently after operative treatment of complex fractures of the distal tibia and ankle (pilon fractures). These are difficult management problems and, even with meticulous technique, are not entirely preventable. Tissue transfer may be needed to obtain adequate soft-tissue coverage in this difficult anatomical area.
Infection
The risk of infection can be decreased with careful attention to the handling of the soft tissues and the technical aspects of internal fixation. The infection rate in treating closed fractures with the current techniques of internal fixation is less than 2%,234,259,270,274 although higher rates of infection with operative treatment have been reported in the past.60,117
The same principles of treating infection after internal fixation in other parts of the skeleton apply to the ankle. Superficial infections may resolve with local wound care and antibiotics. If needed, the incision can be reopened and the wound treated with dressing changes or whirlpool or both. Deep infections require formal exploration and debridement of the joint. The fixation should be left in place if it is stable and the fracture is not healed. Preservation of the joint depends on the organism involved, amount of articular damage present, and response to treatment. Infections with bone involvement and most gram-negative infections require extensive debridement, and an arthrodesis may be required as a salvage procedure.
Arthritis
Degenerative arthritis can result from damage to the articular cartilage at the time of the injury, from altered mechanics of the joint resulting from ligamentous instability or inadequate reduction of the fracture, or from both.18,154,196,234 Anatomical reduction does not totally prevent the development of degenerative changes because blunt injury to the articular surfaces is not correctable. Degenerative changes were reported in about 10% of fractures that were adequately reduced and in 85% of those inadequately reduced; these radiographic changes were usually present within 18 months of injury.196 The incidence of arthritis increases with the severity of the injury.196,234 An increased incidence was also found in older patients, especially in women with osteoporosis. Considering the frequency of ligament and bony injuries involving the ankle, the incidence of degenerative arthritis of the ankle is surprisingly low.
The clinical findings do not always correlate with the radiographic appearance of the joint. For symptomatic arthritis unresponsive to nonoperative modalities, an ankle arthrodesis is the most predictable reconstruction.116
Sympathetic Dystrophy
Reflex sympathetic dystrophy may be seen in all types of ankle injuries. It is characterized by pain out of proportion to the injury, cool and often erythematous or shiny skin, and atrophy of the bone and soft tissues. The symptoms do not decrease within the normal interval of healing. Reflex sympathetic dystrophy may be a component of 'fracture disease' and can be minimized by anatomical restoration of the joint and prompt return to function. It may be a more frequent complication after apparently simple injuries or after prolonged immobilization, but the actual incidence of dystrophy after various types of injuries and methods of treatment is not known.
Treatment is directed at restoration of function and interrupting the pain cycle. Pharmacologic manipulation with intravenous regional corticosteroids or sympathetic blockers, lumbar sympathetic blocks, or calcium channel agents has been reported to be successful.345 As with reflex sympathetic dystrophy elsewhere, the best treatment is prevention with appropriate management of the injury and functional mobilization.
Compartment Syndrome
Compartment syndrome of the foot may occur after injury to the ankle. Direct vascular injury at the ankle is unusual, but vascular compromise can occur from unreduced fracture-dislocations or with associated trauma to the lower leg or foot.376 Early recognition and treatment are needed to prevent the sequelae of decreased sensation and contracted plantar musculature.
Synostosis
Heterotopic bone may form between the distal tibia and fibula after injuries to the syndesmosis. This may vary from a few islands of bone to complete synostosis. Ossification is usually seen at the level of the fibula fracture (see Fig. 31-32C) and often in association with the use of a syndesmotic screw; it is unclear if this results from injury to the syndesmosis or the use of a screw or both.191 A synostosis may interfere with the normal motion and mechanics of the fibula, and patients may sometimes complain of a feeling of stiffness even if they have good ankle motion. A synostosis usually does not require treatment, especially if the ankle has good motion.147,234 In the past, syndesmotic disruption was treated using bone grafts to create a surgical synostosis between the tibia and fibula. These patients were reported to have few problems related to this synostosis, supporting the recommendations for conservative management of this problem. An active patient with a symptomatic synostosis may benefit from excision.268
Osteochondral Fracture
Osteochondral (transchondral) fractures of the talus can occur after any type of injury to the ankle, including 'simple sprains.' They account for only 0.09% of all fractures and 1% of all talus fractures and usually occur on the second through fourth decades of life.350 These fractures can occur on either the lateral or medial side of the talar dome. The lateral lesion is usually associated with a history of trauma. As the talus is forcefully inverted, the lateral edge of the dome shears against the adjacent fibula, creating a shallow, wafer-shaped fracture. These are often more symptomatic and more prone to displacement than the medial lesions (Fig. 31-48). The medial osteochondral lesion is believed to result from impaction of the talus against the tibia, although a definite history of trauma is less common than with lateral lesions. The lesion is usually broader and thicker and less prone to displacement.23
In many cases, the immediate
postinjury x-rays do not reveal evidence of these injuries. Areas of local
compression or fracture may not be detected on plain films, or the fracture may
be anterior or posterior to the dome, requiring plantarflexion or dorsiflexion
of the ankle to be visible on the mortise view. These lesions may heal in
place, remain in place without healing, or detach and become a loose body.6 Chronic pain, swelling, and symptoms of instability may
be present.
The classification system of Berndt and Hardy is the most universally accepted.23 Four stages are described: stage 1 is a small area of compression of the subchondral bone; stage 2 is a partially attached osteochondral fragment; stage 3 is a completely detached but nondisplaced fragment; and stage 4 is a displaced, detached fragment.
The osteochondral defect is usually demonstrated on plain radiographs. An anteroposterior radiograph in plantarflexion increases visualization of the medial dome, and the lateral dome is seen better on a mortise view in dorsiflexion. High-resolution CT scanning, using 2-mm cuts, delineates the dimensions of the lesion and has allowed improvement in definitive staging, particularly between stage 2 and stage 3 lesions.245 The treatment of osteochondral fractures is based on the stability of the fragment, and MRI consistently differentiates between stages 1, 2, and 3. An unstable fragment has synovial fluid or granulation tissue between the fragment and the crater, and MRI is able to demonstrate these findings.195
Treatment is based on the classification of the lesion. Asymptomatic stage 1, 2, and 3 require no treatment. Symptomatic stage 1 or 2 should have a trial of conservative management consisting of activity restriction or immobilization, and those patients with persistent symptoms require surgical treatment. For stage 4 lesions and those unresponsive to immobilization, either reduction and pinning or removal of the fragment with drilling of the defect and early motion is used.350 An anterolateral arthrotomy will usually provide adequate exposure of a lateral lesion, while a medial lesion may require an osteotomy of the medial malleolus.6,61 Arthroscopic treatment of these lesions appears to have comparable results to arthrotomy with less operative morbidity; it may be the preferred method of operative treatment, provided the essential equipment and expertise with ankle arthroscopy is available.16,304,314,382 Lateral lesions are frequently of a higher stage and require surgical treatment more often.
Dislocations of the ankle without fracture are uncommon. Dislocation occurs with a force directed against the plantarflexed foot. The talus is forced out of the mortise, and the loading forces and the position of the foot determine the final direction of displacement.121 A medial or posteromedial dislocation results from a posterior force on the foot (talus) or anterior force on the tibia, followed by axial loading and inversion of the foot. Medial, lateral, posteromedial, posterior, and rotatory dislocation are the most common types.194 Almost half of the reported cases of ankle dislocations were open injuries.194,377,407 Injury to the distal tibiofibular joint appears to be variable; the intact fibula may also be dislocated either posterior or anterior to the tibia.407 There is obviously some overlap between ankle dislocations and tibiofibular diastasis injuries.
The physical findings correlate with the direction of the dislocation. Prominence of the talus and change in the apparent length of the foot are common findings. Neurovascular compromise is uncommon with closed injuries; most injuries to dorsalis pedis or posterior tibial vessels are in open dislocations.
The dislocation should be reduced emergently. Closed reduction using gentle manipulation with appropriate sedation is usually successful. Open reduction may be needed when the fibula is also dislocated. Open injuries require surgical debridement, but reduction of the dislocation should not be delayed unless operative treatment is immediately available. Most authors recommend postreduction immobilization in a cast for 6 to 9 weeks. Good, long-term results have been reported with closed treatment.82,202,348,388,402,407 Residual swelling and some decrease in range of motion are common, but most patients are able to resume their activities, and chronic ligamentous instability is uncommon. Most of the unsatisfactory results occurred in open injuries. There was no difference in outcome between closed treatment and primary ligamentous repair; therefore, the role of ligament repair in these injuries is unclear. Most patients had some late radiographic changes, including ligament calcification, small osteophytes, or articular space narrowing.
Authors' Preferred Method of Treatment
We manage this injury by emergent reduction. Open dislocations are debrided with the same concerns for contamination as in open fractures. The ankle is immobilized in a short-leg cast for about 6 weeks and then is supported by a fracture brace during rehabilitation. Progressive weight bearing is begun according to the patient's symptoms. Repair of the ligaments and capsule is usually performed only if they are easily accessible through the operative wound used for treatment of an open fracture or an irreducible dislocation requiring open reduction.
LIGAMENTOUS INJURIES
Ankle injuries are among the most common problems seen by physicians and in emergency departments. It has been estimated that there is one inversion injury per 10,000 injuries, accounting for a total of 25,000 ankle injuries per day in the United States.1
Ankle sprains are graded depending on injury severity. Grade I involves microscopic stretching or tearing within the ligament substance itself. Grade II injuries involve a gross macroscopic tear of the ligament. Grade III injuries are a complete rupture of the ligament.
Lateral Ligaments
The majority of ankle sprains occur in this complex of ligaments. The sprains are commonly associated with sports activities, especially in the 15- to 35-year-old athlete.36,43
Pathoanatomy
The ligaments that comprise the lateral complex of the ankle consist of the anterior talofibular ligament (ATFL), the posterior talofibular ligament (PTFL), and the calcaneofibular ligament (CFL). The CFL is in intimate association with the peroneal tendon sheath; thus, injuries to the peroneal retinaculum and injuries and dislocations of the peroneal tendons are commonly associated.266,311,357
When the ankle is in a neutral position, the CFL is perpendicular to the long axis of the talus, with its anterior fibers in tension. The ATFL, which is parallel to the long axis of the talus, is not in tension. As the ankle is dorsiflexed, the anterior fibers of the CFL will become taut. As the ankle is plantarflexed, the CFL fibers relax and the ATFL will be in tension.101 Thus, the ATFL and CFL act synergistically.324 The ATFL is a primary stabilizer to ankle inversion in the unloaded plantarflexed position and also has the weakest tensile strength.13 Thus, it is the first ligament to be torn after the lateral capsule.209 The CFL fibers are injured next after a complete tear of the ATFL with a variable injury to the PTFL. However, when the ankle is loaded, stability is significantly enhanced by the interlocking of the ankle articular surfaces themselves.367 When the ankle is loaded in weight bearing, the ankle articular surfaces may contribute up to 30% stability in rotation and 100% stability in version.36 In inversion, the articular contribution on the loaded ankle may be the major resisting force to injury.232
In external rotation, the primary restraint is the CFL, with the PTFL playing a greater role in plantarflexion.232 In the loaded ankle, articular congruity may increase ankle stability by as much as 65%.
Lateral instability may also be caused by damage to the peroneal tendons or their retinaculum, leading to a functional lateral instability.2,140,198,356 Although this is not a common etiology, correct diagnosis of this condition at the time of presentation will alter the patient's treatment and may prevent a lengthy history of instability2,198 and chronic ankle pain.356 The effect of peroneal strength, reaction time, and proprioception has also yet to be completely defined, but peroneal injury is clearly associated with lateral instability.97,188,197
Patient Evaluation
The patient commonly reports an ankle injury while twisting the foot. A pop or sensation of immediate giving way may also be described. Generally, the patient can identify a mechanism or method of injury as well as a direction. Common causes include sporting activities such as running, cutting movements, or jumping, as well as minor trauma such as stepping into a hole or stepping off a curb.
The physical examination will commonly localize pain directly over the ligaments that are injured. Swelling and ecchymosis may also be present. There is generally also increased discomfort with stress of the ankle.
Radiographs include the standard anteroposterior, mortise, and lateral views. These are primarily to aid in identifying an osseous injury such as an avulsion fracture of the base of the fifth metatarsal, an inversion fracture of the anterior process of the calcaneus, an osteochondral fracture of the talar dome, or fracture of the lateral process of the talus or lateral tubercle of the posterior process.146
A stress test may be used to further delineate instability. This includes inversion stress views and anterior drawer stress views. Various authors may use manual testing or use a specific apparatus to create a consistent force to aid in test reproducibility. Also, the amount of instability is dependent on the patient's discomfort, and the level of anesthesia will affect the amount of abnormality exhibited. The anterior drawer test has been used to test the integrity of the ATFL by subluxing the talus anteriorly from the tibia. This may be done manually and the amount of subluxation observed by the physician, or a lateral radiograph may be taken to document the amount of forward subluxation. Jigs are also available to standardize the amount of force used in the test. Normal values range from 2 to 9 mm.35 However, many authors recommend clinical correlation as well as examination and comparison views of the contralateral normal ankle.
The talar tilt test is also a radiologic and clinical examination used for patient evaluation. A forceful inversion stress is applied to the calcaneocuboid or cubotarsal area of the foot. A radiograph is taken, and the angle defined by the tibial plafond and the dome of the talus is measured. Unfortunately, this may be the only point of general agreement. Controversy exists regarding the appropriate knee position43,90,129,143 and the position of the ankle10,25,26,43,105,119,162; if the test should be performed in a jig221 or by a surgeon353 or a trained technician119; and if an anesthetic should be used and, if so, what type.26,89,105,115,119,128,131,132,135,143 Even the amount of normal talar tilt ranges from 5° to 10° of relative talar tilt to 0° to 15° of absolute talar tilt.34,67,199,200
Ankle arthrography may be used to delineate ligament rupture by dye extravasation. The dye should not extravasate beyond the tip of the lateral malleolus or more than 5.5 cm above the tip of the fibula into the peroneal tendon sheath.36 This test has been believed to be more reliable than either the talar tilt test or the anterior drawer test.192
As a diagnostic tool, MRI appears promising. In a study comparing stress radiography with conventional MRI and MR arthrography, Chandnani and coworkers73 reported MR arthrography was 100% accurate, sensitive, and specific in diagnosing ATFL tears and 90% sensitive, 83% specific, and 82% accurate in diagnosing CFL tears. This is in contrast to an ATFL tear diagnosed with MRI alone of 50% sensitivity, 100% specificity, and 59% accuracy. MRI was 50% sensitive, 83% specific, and 63% accurate in the diagnosis of CFL tears. This is in comparison to stress radiography, which was 57% sensitive, 100% specific, and 65% accurate in diagnosing any tear.73 Although the role of MRI has not specifically been defined, it may decrease invasive studies and increase accuracy and specificity of diagnosis while also affording the opportunity to diagnose subchondral or chondral injuries. The cost of this modality remains prohibitive, and its routine use for all ankle injuries is not recommended.
Treatment
Grade I and II injuries occur primarily in the CFL and ATFL. Treatment is generally conservative, and initial management consists of rest, application of ice or cold compresses, elevation of the extremity, and light compression dressing for the initial 24 to 72 hours. Later, early range of motion and splinting with a rigid orthosis, gel cast, air splint, or taping as tolerated by the patient with limitations of activity is done.97 Physiotherapy has generally been advocated, with the literature emphasizing proprioceptive and peroneal strength training before return to sporting activities.36,136
Grade III injuries often reveal a complete rupture of the CFL and the ATFL. It is considered an unstable injury and may be treated in a variety of modalities. Initial conservative management may be performed with immobilization for up to 6 to 8 weeks in a cast.26,52,67,78,89,115,132,133,155,232 Some authors advocate direct repair of active individuals, especially athletes, to avoid problems in the future.149,285,331,363 Other indications for operative intervention may be the presence of a large bony fragment representing an avulsion fracture or a grossly unstable ankle in which both lateral and medial sides of the ankle have been severely compromised, in essence, a dislocation.187 Other authors state that the majority of patients do well with initial conservative care and, if chronic instability results, a later repair or reconstruction will lead to equally as good results as an immediate repair.10,70,115,175,231
Authors' Preferred Method of Treatment
We treat all patients initially with ice and a compressive bulky dressing for soft-tissue control. The patient should be reexamined several days later if an initial diagnosis of the grade of injury was not reached, either due to the severity of symptoms, the delayed time of presentation, or the unreliability of the patient. Patients who have grade I and II injuries are treated with gentle active motion exercises and a functional air or gel cast type of splint. They are restricted from their sports activities until they are fully able to bear weight.
We rehabilitate patients with a combination of range of motion and strengthening exercises concentrating on peroneal function and balance board proprioceptive exercises. We do not allow a return to sports until the patient is able to do proprioceptive functions with side-to-side lateral movements.
In patients who have grade III ankle sprains, we test for functional instability with the talar tilt test and anterior drawer test by clinical examination and with radiologic examination. If the ankle is grossly unstable compared with the normal contralateral side, we immobilize it in a cast for 6 weeks and then begin an aggressive physiotherapy regimen. In the reliable patient, consideration of a walking cast boot is given. All patients may bear weight as tolerated, generally in the range of 2 to 3 weeks after injury. If they are functionally stable, we institute a program similar to the treatment of grade I and II injuries. We reserve operative acute intervention for only those patients who are high performance or professional athletes.
Chronic Lateral Instability
Residual symptoms of pain and instability may be present in up to 20% of patients with ankle ligament injuries.129 Recurrent sprains may lead to elongation and attenuation of the lateral collateral ligaments, chronic instability, and degenerative changes in the joint.97 Changes in joint proprioception and dynamic function of the peroneal muscles may contribute to recurrent injury.36,131,133 Cass and colleagues67 found no difference between the results of early repair and those from late reconstruction. This finding supports nonoperative management of acute injuries because good results can be obtained with reconstruction in the small number of patients who have symptomatic instability. A number of surgical reconstructions have been reported, with good results in more than 90% of patients.78,114,182,322,335,338,351
Injury to the Medial Ligament
This is an uncommon isolated injury but can occur with abduction or external rotational stresses. Injury to the deltoid ligament most commonly occurs with an associated syndesmotic or lateral ankle sprain. These are usually partial tears involving the anterior fibers of the superficial deltoid.
In eversion, the unloaded ankle gains the majority of its stability from the deltoid ligament, with the lateral ankle ligament complex acting together as secondary stabilizers.367 However, in the loaded ankle, the articular surface contact becomes the primary stabilized force and gives up to 100% of the stability in this situation.367 In internal rotation, the two primary restraints are the ATFL and the deltoid ligament,367 but their individual contribution to stability is dependent on position and load of the ankle.
An isolated deltoid ligament injury should be treated nonoperatively. Adhesive taping, bracing, and casting have all been used with satisfactory results.
Authors' Preferred Method of Treatment
If there is no evidence of lateral subluxation of the talus, deltoid sprains are managed by immobilization in a fracture brace or cast, followed by rehabilitation, with emphasis on the inverting muscles of the foot, particularly the tibialis posterior muscle. Bracing and rehabilitation continue for 6 weeks, and the patient is allowed to resume normal activities once adequate strength and flexibility has been obtained.
Syndesmotic Ligament Disruption
Complete rupture of the syndesmotic ligaments (diastasis of the tibia and fibula) in the absence of fracture is rare.59,112,254 In a study of US Military Academy cadets, of 1344 ankle sprains, only 15 were syndesmotic injuries.167 The most common mechanism of injury appears to be associated with external rotation of the foot.167,320 Most often, the anterior tibiofibular ligament is involved alone.146 In the more severe injuries where a frank diastasis is noted, the interosseous ligament and the posterior tibiofibular ligaments are ruptured as well, with the deltoid ligament occasionally involved.146
Patients report pain and swelling in the anterolateral aspect of the ankle. Tenderness of the anterior tibiofibular syndesmosis is present, and palpation proximally may also reveal extension of the injury into the syndesmosis itself. The patient's symptoms should be exacerbated by external rotation or dorsiflexion of the foot. Hopkinson and associates167 described a squeeze test by compressing the tibia and fibula together midway down the calf. It is positive when proximal compression elicits distal pain in the area of the syndesmotic and interosseous ligaments.
Edwards and DeLee112 have described two types of diastasis. In a latent diastasis the x-rays appear normal and widening of the mortise is seen only on stress x-rays. A frank diastasis is easily seen on routine films. In a frank diastasis the fibula may be normal or plastically deformed so that an osteotomy of the fibula is needed to reduce the ankle.112 Unless properly managed, chronic pain, swelling, and instability may be a problem. A later radiographic finding may include ossification of the interosseous membrane several weeks after injury167 when the clinician first may be made aware of this injury. The immediate treatment of this injury is rest, application of ice packs, and elevation and splinting of the extremity. Gustilo and colleagues146 treat these injuries with cast immobilization and non-weight bearing until no tenderness may be elicited in the anterior tibiofibular ligament with palpation or foot dorsiflexion. This generally occurs 2 to 4 weeks after injury. Other authors have used a regimen of crutches with non-weight bearing until standing and toe-raising are not painful and then convert to a functional ankle brace.232
Authors' Preferred Method of Treatment
Conservative treatment of this injury as outlined earlier is instituted when an incomplete injury occurs. If a complete rupture of the syndesmotic ligaments is present, we believe it should be managed by operative repair of the ligaments, by stabilization of the fibula to the tibia with a syndesmotic screw, or by both.
|
Politica de confidentialitate |
| Copyright ©
2026 - Toate drepturile rezervate. Toate documentele au caracter informativ cu scop educational. |
Personaje din literatura |
| Baltagul – caracterizarea personajelor |
| Caracterizare Alexandru Lapusneanul |
| Caracterizarea lui Gavilescu |
| Caracterizarea personajelor negative din basmul |
Tehnica si mecanica |
| Cuplaje - definitii. notatii. exemple. repere istorice. |
| Actionare macara |
| Reprezentarea si cotarea filetelor |
Geografie |
| Turismul pe terra |
| Vulcanii Și mediul |
| Padurile pe terra si industrializarea lemnului |
| Termeni si conditii |
| Contact |
| Creeaza si tu |